Pre- and post-operative patient care for transoral thyroidectomy
Introduction
A new surgical technique when developed has to maintain or advance to its conventional standard and be at least comparable when it comes to results achieved, complications, safety, technical feasibility and cost-to-benefit ratio by the open tradition surgery (1).
A considerable development has occurred in the application of endoscopic techniques in thyroid surgery (2).
Gagner and Hüscher first reported successful endoscopic neck surgery in 1996 and 1997 (3). About 20 different endoscopic thyroid surgical techniques have been developed (4).
Minimizing surgical stress, cosmetic concerns and improving the postoperative quality of life are the main motivations for developing novel endoscopic thyroid surgical techniques (5).
According to the insertion site of surgical instruments, endoscopic surgery can be classified as cervical, anterior chest wall, breast, axillary, axillary breast approaches and transoral via vestibular incision (6-8).
Here we denote not going into the technical description of the surgical procedure, but instead highlighting some of the pre- and post-operative aspects of transoral endoscopic thyroidectomy vestibular approach (TOETVA) in patient management (8-13).
Pre-operative peculiarities
Inclusion and exclusion criteria
The results of previous reports and studies on TOETVA support the importance of careful selection of Patients for outcome measures and the impact that precise Patient candidacy and safety have on outcome. The patient selection criteria must be observed strictly to maintain TOETVA safety. The inclusion and exclusion criteria used for TOETVA are summarized in Tables 1 and 2. Relative contraindication are obesity or not too short neck, ASA 3, and contraindication for nasotracheal intubation.
Table 1
| TOETVA may be indicated if the conditions mentioned below are found |
| • Predicted gland width on diagnostic imaging ≤10 cm |
| • Thyroid volume outline of <45 mL |
| • Dominant nodule dimension of ≤50 mm |
| • Bethesda 3 and 4 lesions |
| • Primary papillary microcarcinoma without local or distant metastasis |
| • Patient request for optimal aesthetic results |
TOETVA, transoral endoscopic thyroidectomy vestibular approach.
Table 2
| TOETVA must not be indicated |
| • Patients unfit for general anesthesia |
| • Precedent radiation in the head, neck, upper mediastinum |
| • Antecedent neck surgery |
| • Recurrent goiter |
| • Main nodule diameter of >50 mm |
| • Gland volume of >45 mL |
| • Documentation of lymph node |
| • Distant metastases |
| • Tracheal/esophageal infiltration |
| • Preoperative laryngeal nerve palsy |
| • Hyperthyroidism |
| • Mediastinal goiter |
| • Oral abscess |
| • Patients with poorly- or un-differentiated cancer |
| • Dorsal extrathyroidal tumor |
| • Lateral neck metastasis |
TOETVA, transoral endoscopic thyroidectomy vestibular approach.
Furthermore, it is important to specify that male patients are more challenging for TOETVA because: (I) chin to neck region step is more challenging because, more of robust tissues; (II) laryngeal prominence/thyroid cartilage is larger in adult men and interferes with vision, interferes with instrumentation.
Preoperative imaging
All patients are evaluated pre-operatively using ultrasonography, and fine-needle aspiration cytology. Imaging is essential to identify the proper patient for TOETVA and for the beginner surgeon. Imaging should demonstrate an uncomplicated thyroid nodule. Preoperative US is mandatory, with evaluation of the following three proper “s” site, size and shape (oval). Nodule size means: (I) not to small and not too big; (II) 3 cm nodule is appropriated; (III) easy to see endoscopically; (IV) it isn't difficult to dissect; (V) it isn't too hard to handle when you look for the RLN; (VI) it isn't too complicated to put the nodule into the endobag and removed from the vestibule. Proper location means: (I) not too low (near the suprasternal notch); (II) not too high (upper pole dissection); (III) it should be not too deep (posterior lobe), not adhere carotid sheath, hide underneath SCM or difficult to palpate
Pre- and post-operative laryngoscopy
All patients undergo pre-operative direct laryngoscopy to assess vocal cord motility. TOETVA is still in the development phase, that is why laryngoscope is mandatory, for auditing.
Surgeon candidacy
For the general surgeon, it is important that he has wide experience in open thyroid surgery, training in endoscopic thyroidectomy (ET), familiarity in laparoscopy (i.e., retroperitoneal). For the head and neck surgeon a wide experience in open thyroid surgery, has trained in ET, familiarity in endoscopy (i.e., sinus surgery). The surgeons should have essential anatomy of the oral cavity (lip and chin), how to protect the mental nerve, of course of the neck anatomy, how to identify and protect RLN and parathyroid gland, etc. To be considered by the Surgeon that a left lobectomy is more challenging for the right hand surgeon, instruments interbreed, and again (in male patient) laryngeal prominence. Right hand surgeon should start operate with right thyroid nodule (i.e., right lobectomy, female).
Assistant and nurse
The 1st assistant is important (Figure 1): (I) helps to hold correctly the camera; (II) key person to help endoscopic surgery become a success; (III) well informed/knowledgeable; (IV) clearly understand all steps of operation; (V) to be able to read surgeon’s mind; (VI) fluent and active.

Surgical anatomy
Transoral thyroidectomy is performed with a cranial to caudal view and cranial to caudal dissection. If in open surgery, the surgeon usually performs caudal to cranial procedure, the Authors suggest to change the view point by standing during open surgery at patient head and make cranial to caudal dissection and start and learn to locate RLN at its entry point first.
Dental care
Before starting your first trans oral case interact and discuss with your dental specialist.
Oral microbiology includes anaerobic bacteria: Actinomyces, Arachnia, Bacteroides, Bifidobacterium, Eubacterium, Fusobacterium, Lactobacillus, Leptotrichia, Peptococcus, Peptostreptococcus, Propionibacterium, Selenomonas, Treponema, and Veillonella.
Genera of fungi that are frequently found in the mouth: Candida, Cladosporium, Aspergillus, Fusarium, Glomus, Alternaria, Penicillium and Cryptococcus.
A highly efficient innate host defense system constantly monitors the bacterial colonization and prevents bacterial invasion of local tissues.
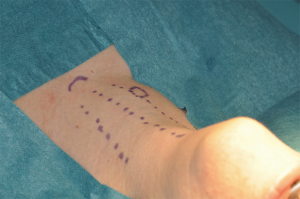
However, the 3 vestibular incisions determine a new communication between the oral cavity and neck and a poor oral heath may contribute the ability of the oral microbiota to invade the body (Figures 2-4). Good oral and dental hygiene can prevent possible postoperative infective complications. Therefore, it is suggested a preoperative oral/dental assessment by specialist. Patients undergo dental care about 1 month before TOETVA. This is recommended especially in high risk subjects as diabetic and cardiovascular patients. Moreover, pre- and post-operatively, patients are asked to gargle with Chlorhexidine mouth wash. Amoxicillin/clavulanic acid is used for preoperative prophylactic antibiotic. Some authors suggest extending the antibiotic for 5 days postoperatively orally
Post-operative peculiarities
Table 3 summarize postoperative care for TOETVA patients.
Table 3
| Postoperative management |
| Oral antibiotics for 5–7 days. Some authors suggest only intraoperative prophylaxis |
| No dressing is required. Some authors suggest a compression dressing applied to the anterior neck for 12–24 hrs |
| Mouthwash 3 times per day for 5–7 days. Brushing teeth from 1st day post-op. |
| Oral diet on day 0 postoperatively (evening) |
| Patients are mobilized from bed 4hrs postoperatively |
| Patients can take a shower and man shave on day 0 postoperatively (evening) |
| Patients can sunbathe on the following weekend |
TOETVA, transoral endoscopic thyroidectomy vestibular approach.
Oral antibiotics are continued for 5–7 days, but some Authors suggest only intraoperative prophylaxis. Dressing is not required. Some Authors suggest a compression dressing applied to the anterior neck for 12–24 hrs. Mouthwash is suggested 3 times per day for 5–7 days (1,13).
Brushing teeth from 1st day post-operatively. Oral diet is started on day 0 postoperatively (evening).
Patients are mobilized from bed 4hrs postoperatively. Patients can take a shower and man shave on day 0 postoperatively (evening). Patients can sunbathe on the following weekend (1-13).
Discharge
Discharge is guided by the common rules of the thyroid surgery, after careful evaluation by surgeon, endocrinological and anesthesiological specialist, serum calcium dosage and after neck, mouth and postoperative laryngeal evaluation (2,3). Patient is follow-up in clinics.
Follow-up
Follow-up examination included hoarse voice, swallowing difficulty, hypesthesia or paresthesia and cosmetic satisfaction. The patients are asked to grade the cosmetic appearance after surgery (4). All patients are commonly provided with four ratings of cosmetic satisfaction: poor, acceptable, good and excellent. Figure 5 depict the outcomes of the cosmetic results at the vestibule area and neck.

To avoid the formation of adhesions, patients are invited to begin massaging the lower lip, the chin, the neck, with rotary massages already from the 5th postoperative day, sliding the skin on the deeper levels. Patients are also invited to move the neck, extending it upwards and sideways, also to avoid adhesions.
Conclusions
Patient selection is the process by which an evaluating surgeon decides whether to accept responsibility for the care and treatment of a potential patient with new approach. It is assumed the physician has the requisite knowledge to assess the anatomic disorder and the new technical ability to render appropriate care if needed.
In this report we tried to highlight the importance of patient selection in avoiding complications and achieving outcomes comparable to open procedures. The aim of this report is to help the less experienced surgeon initiated to TOETVA. An unsatisfactory outcome can be measured not only by failure to resolve the disorder but also by expenditure of a disproportionate amount of practice resources in achieving resolution of the thyroid problem.
Thyroid surgeons have started performing increasingly complex procedures involving tumor resection, prophylactic node dissection, endoscopic or robotic surgery as the TOETVA (2).
Cosmetic thyroid surgery is rapidly becoming a common issue in a busy endocrine surgery practice. Improving cosmetic outcomes have been a direct and logical derivative of technical advances, minimally invasive and endoscopic approaches, societal and cultural needs (6). Avoidance of cervical incision is important to many individuals, not limited to models, and woman (4).
When aesthetically pleasing thyroidectomy can be performed without compromising surgical goals and patient safety, cosmesis in 2018, is a factor in the presurgical planning and discussion with Patients (7).
Endocrine surgeons while gain experience, focus and emphasize on cosmetic outcomes (8).
TOETVA is a new technique that demands perfect patients’ candidacy and preparation, intraoperative full control of laryngeal nerves function and parathyroid glands, and best follow-up 9, 10).
Surgeons cannot apply a new approach without perfect precise pre- and post-operative management of TOETVA patients. This would be in contrast with commonly performed routine open surgery. It would be a step back in endocrine surgery (2).
Endoscopy and robotic approaches have to be in the same security area of open procedure.
Endoscopy requires auditing to achieve net benefit of the minimally invasive approach.
The same concerns are for any other new technique and technology applied for thyroid and parathyroid operations (13).
Transoral thyroid surgery is new NOTES approach for thyroid gland, and quite feasible. Transoral thyroidectomy would be enhanced to the ideal procedure with specific instrumental and technical developments (11).
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Anuwong Angoon, Hoon Yub Kim, Ralph P. Tufano and Gianlorenzo Dionigi) for the series “Transoral Thyroidectomy” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2018.01.01). The series “Transoral Thyroidectomy” was commissioned by the editorial office without any funding or sponsorship. Gianlorenzo Dionigi served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Thyroid from Mar. 2017 to Feb. 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the manuscript and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chai YJ, Kim HY, Kim HK, et al. Comparative analysis of 2 robotic thyroidectomy procedures: Transoral versus bilateral axillo-breast approach. Head Neck 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Dionigi G, Tufano RP, Russell J, et al. Transoral thyroidectomy: advantages and limitations. J Endocrinol Invest 2017;40:1259-63. [Crossref] [PubMed]
- Dionigi G, Chai YJ, Tufano RP, et al. Transoral endoscopic thyroidectomy via a vestibular approach: why and how? Endocrine 2017; [Epub ahead of print]. [PubMed]
- Chai YJ, Chung JK, Anuwong A, et al. Transoral endoscopic thyroidectomy for papillary thyroid microcarcinoma: initial experience of a single surgeon. Ann Surg Treat Res 2017;93:70-5. [Crossref] [PubMed]
- Russell JO, Clark J, Noureldine SI, et al. Transoral thyroidectomy and parathyroidectomy - A North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol 2017;71:75-80. [Crossref] [PubMed]
- Kim HY, Chai YJ, Dionigi G, et al. Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surg Endosc 2018;32:688-94. [Crossref] [PubMed]
- Anuwong A, Sasanakietkul T, Jitpratoom P, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA):indications, techniques and results. Surg Endosc 2018;32:456-65. [Crossref] [PubMed]
- Anuwong A, Kim HY, Dionigi G. Transoral endoscopic thyroidectomy using vestibular approach: updates and evidences. Gland Surg 2017;6:277-84. [Crossref] [PubMed]
- Dionigi G, Lavazza M, Wu CW. Set al. Transoral thyroidectomy: why is it needed? Gland Surg 2017;6:272-6. [Crossref] [PubMed]
- Dionigi G, Bacuzzi A, Lavazza M, et al. Transoral endoscopic thyroidectomy: preliminary experience in Italy. Updates Surg 2017;69:225-34. [Crossref] [PubMed]
- Dionigi G, Lavazza M, Bacuzzi A, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): From A to Z. Surg Technol Int 2017;30:103-12. [PubMed]
- Dionigi G, Bacuzzi A, Lavazza M, et al. Transoral endoscopic thyroidectomy via vestibular approach: operative steps and video. Gland Surg 2016;5:625-7. [Crossref] [PubMed]
- Dionigi G, Rovera F, Boni L. Commentary on transoral access for endoscopic thyroid resection: Witzel K, von Rahden BH, Kaminski C, Stein HJ (2008) Transoral access for endoscopic thyroid resection. Surg Endosc 22(8):1871-1875. Surg Endosc 2009;23:454-5; discussion 456. [Crossref] [PubMed]
Cite this article as: Navarra G, Bartolo V, Rizzo AG, Marullo M, Cancellieri A, Catalfamo A, Pergolizzi FP, Melita G, Dionigi G. Pre- and post-operative patient care for transoral thyroidectomy. Ann Thyroid 2018;3:3.