
Anesthesiologist perspectives for the transoral approach
Introduction
Thyroidectomy is the most frequently performed endocrine surgery in the United States (1).
Recently, numerous measures aim to improve surgical quality of care, decreasing patients discomfort, surgical invasiveness, intra and postoperative complications. New surgical approaches, including minimally invasive surgery and considerable aesthetic results are pursued (2). In this perspective, endoscopic approaches have been developed and clinically tested, gaining popularity. However, the literature on this topic revealed some controversial aspects concerning intraoperative complications and postoperative pain management (3,4).
In the last few years a new endoscopic technique has appeared in the scenery of thyroid surgery. The transoral endoscopic thyroidectomy vestibular approach (TOETVA) (5) involves the insertion of several optics and instruments through three small incisions on the lower lip vestibule; the subsequent insufflation of carbon dioxide ensures the creation of a wide operative field.
The transoral approach is performed in only few centres around the world; for this reason, it’s difficult to compare this technique to the classical open approach.
The main complications developed after an open thyroidectomy are bleeding, recurrent laryngeal nerve lesions and secondary lesions of the surgical wound (6). The transoral technique may present further complications, as subcutaneous emphysema of the neck and hypercarbia due to carbon dioxide insufflation.
Transoral thyroidectomy complications are summarized in Table 1. These data are obtained from case reports and small sample size trials currently available. The most frequent complication is the recurrent laryngeal nerve lesion followed by subcutaneous bleeding. The subcutaneous emphysema may also extend to the thorax and the mediastinum when carbon dioxide is inflated with excessively high pressure (7,20).
Table 1
| Authors | N | Surgical complications |
|---|---|---|
| Wilhelm and Metzig (7) | 8E | 1 TRLNP |
| 1 PRLNP | ||
| 1 “small mediastinal emphysema” | ||
| Wang et al. (8) | 10 | – |
| Yang et al. (9) | 6 | – |
| Sasanakietkul et al. (10) | 12P | 1 TRLNP |
| Chand and Mishra (11) | NS | – |
| Jitpratoom et al. (12) | 46 | 4 TRLNP |
| 1 conversion to open surgery due to an “unstoppable bleeding” | ||
| Anuwong (13) | 60 | 2 TRLNP |
| 1 “late hematoma” | ||
| Park et al. (14) | 1 | – |
| Dionigi et al. (15) | 1 | – |
| Pai et al. (16) | 1 | 1 “mild emphysema” in the neck area |
| Zeng et al. (17) | 4 | – |
| Lee et al. (18) | 4D | – |
| Udelsman et al. (19) | 5 + 2P | – |
| Nakajo et al. (20) | 8 | 1 PRLNP |
| Yang et al. (21) | 60 | 2 “mandibular subcutaneous bleeding” |
| Anuwong et al. (22) | 200 | 8 TRLNP |
| 3 “mental nerve injury” | ||
| 1 “post-operative hematoma that required open surgery” |
P, parathyroidectomy; E, enzyme multiplied immunoassay (eMIT) technique. D, da Vinci robotic system. TRLNP, transient recurrent laryngeal nerve palsy; PRLNP, permanent recurrent laryngeal nerve palsy; NS, not specified.
In this manuscript we describe the anaesthetic perspectives on transoral thyroidectomy performed in our centres, focusing on the preoperative, intraoperative and postoperative phases. Endoscopic techniques on neck are gaining clinical success and the anaesthetists involved in patient care have to be aware of the main challenging aspects.
Preoperative management
During the preoperative phase the anaesthetists should focus on standard cardio respiratory function, highlighting potential thyroid-related upper airway obstructive symptoms. For this reason, in addition to routine preoperative exams a lateral neck and chest X-ray may be requested and in selected cases a CT scan may be performed (23). Preoperative airway evaluation follows the usually validated score (24). The naso-tracheal intubation, if requested, should be cautiously managed in patients with nose defects; for this reason, an ear, nose and throat (ENT) preoperative evaluation including a fiberoptic visualization of nose and pharynx tract may be diriment.
Identification of hypo or hyperthyroidism is useful to treat in advance uncontrolled metabolic state and prevent potentially catastrophic perioperative emergencies (25).
Intraoperative management
Before anaesthesia induction all patients have to be monitored according to the standard practice (26). In several cases is recommendable to proceed with invasive arterial monitoring to visualize the real-time blood pressure value and to analyze blood gases. A central venous catheter is rarely needed; in selected cases the femoral approach is recommended. We prefer to avoid a neck venous access due to surgical comfort and also to preserve the anatomic structure avoiding all possible preoperative injury might undercut the surgical success. Additionally, if any intraoperative accident occurs, the blood flow to superior vena cava could be lowered.
Surgery is performed under general anesthesia, requiring nasal or oral intubation. The nasal intubation is related with possible sinus trauma with secondary bleeding (27). We routinely use endotracheal lidocaine instillation before tracheal tube placement to reduce curare dose and to prevent cough reflex during intubation (28). Local anaesthetic use does not affect the effectiveness of intraoperative neuromonitoring (IONM) procedure (29).
Total intravenous anesthesia (TIVA) is the more suitable technique for this surgery in order to obtain a stable anesthetic plan with a minimal impact on (IONM and a rapid onset and recovery thanks to pharmacokinetics propriety of anaesthetic drugs. The use of nitrous oxide (N2O) is contraindicated for possible operative field distension and mainly for postoperative nausea and vomiting (PONV) onset (30).
The tracheal tube should be fixed with an appropriate system and positioned at the same side of ventilator in according with the surgeon.
We usually perform a standardized anesthetic technique with bolus dose of propofol (2 mg/kg) followed by infusion and remifentanil infusion rate (0.2–0.5 γ/kg/min) according to bispectral index (BIS) monitoring system; a single dose of curare could be used to facilitate tracheal intubation.
All anticipated or unanticipated difficult tracheal intubation have to be managed according to guidelines considering that awake fiberoptic intubation is the more effective technique for predictable difficult airways cases (24,31).
During TOETVA, CO2 insufflation is used to create an unnatural working space causing possible deleterious events such as pneumothorax and pneumomediastinum. When cardiovascular instability and respiratory impairment are manifested the risk of cardiovascular collapse is imminent. Therefore, the anaesthetist must supervise the inspired fraction of oxygen, end-tidal CO2, tidal volume, airway pressures and cardiovascular state (32) of the patient.
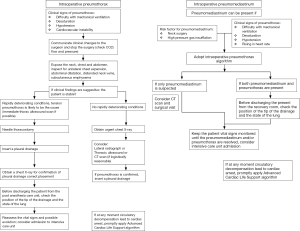
If a surgical complication is suspected the anaesthetist must advise the surgeon and alerts all surgical equipe. Figure 1 shows the main concerns about intraoperative suspicion of pneumothorax or pneumomediastinum. The surgeon, according to previous case reports (2,13,15), should set the pressure insufflation not above 6 mmHg and a flow rate of 15 L/min (temporary increased up 20 L/min). All changes about flow and pressure rate should be reported to all surgical team. The anaesthetist should inform the surgeon about a raising of end tidal CO2 (EtCO2) and subsequently the flow rate should be reduced. The return to physiological EtCO2 values allows to continue with the procedures, conversely is mandatory to stop the flow rate and consider another surgical technique.
Postoperative management
The main complications after thyroidectomy are hypoparathyroidism, recurrent laryngeal palsy and hemorrhage (6). The incidence of hypoparathyroidism is estimated from 0.5% to 65%; however, more realistic data assess a lower incidence of this complication thanks to new measures for improvement of surgical quality (33).
Severe hypocalcemia may appear with cardiovascular instability and laryngeal spasms. In this serious scenario intravenous calcium in addition to oral therapy is tested as resolutive; an appropriate intravenous calcium intake, a premature airway management and advanced cardiovascular therapy are the main goals.
Recurrent laryngeal nerve lesions have an incidence of 9.8% during postoperative period and the bilateral lesion related to severe airway obstructive symptoms is a rare complication (0.4%) (33). Therefore, in few cases reintubation is necessary, considering emergency tracheostomy only as desperate measure. It is recommended to extubate the patients with all surgical team alert and to inform immediately the surgeon about reintubation necessity. In case of reintubation antiedema therapy and a close monitoring on Intensive Critical Care Unit are necessary.
The hematoma onset in the immediate postoperative phase after thyroidectomy with breathing difficulties is a life-threatening emergency (6,34,35). Its treatment consists of airway protection through tracheal intubation as priority and immediate surgical decompression and identification of the bleeding source. The major risk of bleeding is seen during the first postoperative hours; accurate monitoring on the Post Anesthesia Care Unit (PACU) in the subsequent four hours until achievement of discharge criteria is recommended.
Gas insufflation related emergencies are rarely seen. After TOETVA subcutaneous emphysema might be described; this palpable crepitus under the skin is not rare and should not alarm the physicians. All patients with clinical confirmed emphysema have to be closely monitored on the PACU. An oxygen supply should be given to facilitate respiratory activity and carbon dioxide removal. A conservative management is mandatory with a close vigilance on alarming signals such as dyspnea and cardiovascular instability. Asymptomatic patients could be discharged without any further indications.
Pain management
The postoperative pain management after TOETVA is still debated (36). The endoscopic procedures provide better postoperative pain control but despite their benefits, inflammatory process and nerve injury could involve nociceptive and neuropathic pain components. Actually, the expected pain for thyroidectomy is lower than other neck and head surgical procedures but the main challenge is to guarantee an optimal analgesia during speech, chewing and swallowing on postoperative period (22). For these reasons is recommendable to proceed with a multimodal pain control approach with central analgesics such as paracetamol, non-steroidal drugs and opioids.
Recently, Jitpratoom et al. (12) published a comparison between open thyroidectomy and transoral approach and showed a better pain control in the endoscopic group. Although the pain score at day 0 was not reported, we sustain its results.
It is our common practice to administer intraoperative paracetamol dose, endovenous morphine and in selected patients nonsteroidal inflammatory drugs. During early postoperative period it is necessary to avoid excessive cough and unpleasant airway constriction sensation due to endotracheal tube and surgical trauma therefore we recommend an appropriate monitoring on a postoperative unit to treat possible uncontrolled pain.
Conclusions
TOETVA is a recent surgical procedure and for the anaesthetists the CO2 insufflation closer to airway structures represents a challenge. A close cooperation between surgeon and anaesthetist is necessary to avoid serious events. Adequate setting of CO2 insufflation represents the only way to reduce subcutaneous emphysema and related complications. The anaesthetist should alert immediately the surgical team about incoming intraoperative issues and apply shared emergencies protocol. During the preoperative period the anaesthetic alerts are directed to the airway management. In the postoperative phase a conservative approach to subcutaneous emphysema is recommended with constant attention on any vital signs change and evolutive problems.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Anuwong Angoon, Hoon Yub Kim, Ralph P. Tufano and Gianlorenzo Dionigi) for the series “Transoral Thyroidectomy” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2018.04.01). The series “Transoral Thyroidectomy” was commissioned by the editorial office without any funding or sponsorship. Gianlorenzo Dionigi served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Thyroid from Mar 2017 to Feb 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the manuscript and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sosa JA, Wang TS, Yeo HL, et al. The maturation of a specialty: Workforce projections for endocrine surgery. Surgery 2007;142:876-83. [Crossref] [PubMed]
- Dipankar S. Review Article on Transoral Endoscopic Thyroid Surgery. Open Access J Surg 2017;2:555590.
- Karakas E, Steinfeldt T, Gockel A, et al. Transoral parathyroid surgery—a new alternative or nonsense? Langenbecks Arch Surg 2014;399:741-5. [Crossref] [PubMed]
- Slater B, Inabnet W. Pneumothorax: An Uncommon Complication of Minimally Invasive Parathyroidectomy. Surg Laparosc Endosc Percutan Tech 2005;15:38-40. [Crossref] [PubMed]
- Wilhelm T, Wu G, Teymoortash A, et al. Transoral endoscopic thyroidectomy: current state of the art—a systematic literature review and results of a bi-center study. Transl Cancer Res 2016;5:S1521-30. [Crossref]
- Meltzer C, Klau M, Gurushanthaiah D, et al. Risk of Complications after Thyroidectomy and Parathyroidectomy: A Case Series with Planned Chart Review. Otolaryngol Head Neck Surg 2016;155:391-401. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Wang Y, Yu X, Wang P, et al. Implementation of Intraoperative Neuromonitoring for Transoral Endoscopic Thyroid Surgery: A Preliminary Report. J Laparoendosc Adv Surg Tech A 2016;26:965-71. [Crossref] [PubMed]
- Yang K, Ding B, Lin C, et al. The Novel Transvestibule Approach for Endoscopic Thyroidectomy: A Case Series. Surg Laparosc Endosc Percutan Tech 2016;26:e25-8. [Crossref] [PubMed]
- Sasanakietkul T, Jitpratoom P, Anuwong A. Transoral endoscopic parathyroidectomy vestibular approach: a novel scarless parathyroid surgery. Surg Endosc 2017;31:3755-63. [Crossref] [PubMed]
- Chand G, Mishra SK. Transoral Endoscopic Thyroid Surgery through Vestibular Approach. World J Endoc Surg 2016;8:179-82.
- Jitpratoom P, Ketwong K, Sasanakietkul T, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves' disease: a comparison of surgical results with open thyroidectomy. Gland Surg 2016;5:546-52. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Park JO, Kim MR, Kim DH, et al. Transoral endoscopic thyroidectomy via the trivestibular route. Ann Surg Treat Res 2016;91:269-72. [Crossref] [PubMed]
- Dionigi G, Bacuzzi A, Lavazza M, et al. Transoral endoscopic thyroidectomy via vestibular approach: operative steps and video. Gland Surg 2016;5:625-7. [Crossref] [PubMed]
- Pai VM, Muthukumar P, Prathap A, et al. Transoral endoscopic thyroidectomy: A case report. Int J Surg Case Rep 2015;12:99-101. [Crossref] [PubMed]
- Zeng YK, Li ZY, Xuan WL, et al. Trans-oral glasses-free three-dimensional endoscopic thyroidectomy-preliminary single center experiences. Gland Surg 2016;5:628-32. [Crossref] [PubMed]
- Lee HY, You JY, Woo SU, et al. Transoral periosteal thyroidectomy: cadaver to human. Surg Endosc 2015;29:898-904. [Crossref] [PubMed]
- Udelsman R, Anuwong A, Oprea AD, et al. Trans-oral Vestibular Endocrine Surgery: A New Technique in the United States. Ann Surg 2016;264:e13-6. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Yang W, Wang C, Li J, et al. Transoral-vestibule endoscopic thyroidectomy: a novel surgical approach with 3 year experience. J Am Coll Surg 2015;221:e82. [Crossref]
- Anuwong A, Sasanakietkul T, Jitpratoom P, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc 2018;32:456-65. [Crossref] [PubMed]
- Perros P, Boelaert K, Colley S, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81:1-122. [Crossref] [PubMed]
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013;118:251-70. [Crossref] [PubMed]
- Satoh T, Isozaki O, Suzuki A, et al. Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr J 2016;63:1025-64.
- Checketts MR, Alladi R, Ferguson K, et al. Recommendations for standards of monitoring during anaesthesia and recovery 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia 2016;71:85-93. [Crossref] [PubMed]
- Gold M, Pearlman A, Boyack I. Middle turbinectomy after nasotracheal intubation. Emerg Radiol 2016;23:203-5. [Crossref] [PubMed]
- Rabold M, Tintinalli J. Tracheal lidocaine stops airway hyperresponsiveness. Ann Emerg Med 1995;25:432. [Crossref] [PubMed]
- Chu KS, Wu SH, Lu IC, et al. Feasibility of intraoperative neuromonitoring during thyroid surgery after administration of nondepolarizing neuromuscular blocking agents. World J Surg 2009;33:1408-13. [Crossref] [PubMed]
- Visser K, Hassink EA, Bonsel GJ, et al. Randomized controlled trial of total intravenous anesthesia with propofol versus inhalation anesthesia with isoflurane-nitrous oxide: postoperative nausea and vomiting and economic analysis. Anesthesiology 2001;95:616-26. [Crossref] [PubMed]
- Srivastava D, Dhiraaj S. Airway management of a difficult airway due to prolonged enlarged goiter using loco-sedative technique. Saudi J Anaesth 2013;7:86-9. [Crossref] [PubMed]
- Phillips S, Falk GL. Surgical tension pneumothorax during laparoscopic repair of massive hiatus hernia: a different situation requiring different management. Anaesth Intensive Care 2011;39:1120-3. [PubMed]
- Cannizzaro MA, Lo Bianco S, Picardo MC, et al. How to avoid and to manage post-operative complications in thyroid surgery. Updates Surg 2017;69:211-5. [Crossref] [PubMed]
- Lang BH, Yih PC, Lo CY. A review of risk factors and timing for postoperative hematoma after thyroidectomy: is outpatient thyroidectomy really safe? World J Surg 2012;36:2497-502. [Crossref] [PubMed]
- Bacuzzi A, Dionigi G, Del Bosco A, et al. Anaesthesia for thyroid surgery: perioperative management. Int J Surg 2008;6:S82-5. [Crossref] [PubMed]
- Anuwong A. Post-operative pain control protocol for transoral endoscopic thyroidectomy vestibular approach (TOETVA) Gland Surg 2017;6:422-3. reply. [Crossref]
Cite this article as: Bacuzzi A, Guzzetti L, Dionigi G, Menegaldo L, Alicino V, Zanghì GN, Freni F, Cuffari S. Anesthesiologist perspectives for the transoral approach. Ann Thyroid 2018;3:11.


