Trans-axillary intra-operative ultrasound cystic drainage and thyroid lobectomy: a new endoscopic approach
Introduction
Thyroid disease affects one million Portuguese and 30 million Europeans. Up to 70% of adult people are ultrasound positive when evaluated (1,2). Women are five times more likely to suffer from the disease than men (3). Therefore, this is a worldwide health problem (3,4), and, even with more recent thyroid sparing guidelines, many of these patients will nonetheless need surgical intervention.
Remote endoscopic thyroid surgery has spread in Southeast Asia for cultural reasons. In Europe only a few groups are performing these techniques, although there is a growing interest in the population. The reasons for this approach are aesthetic, to avoid stigmatization.
In a world where image takes the front line, the risks of a cervical scar and the impact in social and professional lives are not negligible.
Our group has been performing trans-axillary cervical surgery since November 2014, and we have done 51 procedures so far, including lobectomies, total thyroidectomies and parathyroidectomies.
The series presented in this paper includes three cases of cystic-solid lesions approached with the advent of intra-operative ultrasound (IOUS) to characterize and guide-drainage after lobe dissection.
To our knowledge, there is no previous report on this approach.
The aim of this article is to call attention to endoscopic thyroid surgery and its multiple applicability, as well as to show the aid of IOUS support whenever dealing with voluminous complex cystic-solid lesions.
Operative technique
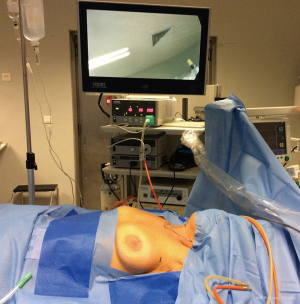
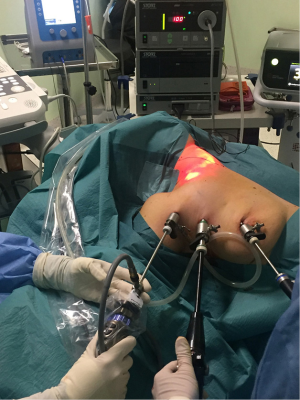
The patient lays on dorsal decubitus with the ipsilateral arm abducted. Two port incisions are made in the armpit on the anterior axillary line and a third one on the nipple border (Figure 1). The lateral ports are 5 mm in diameter and the middle one is a 10 mm for a 0º scope.
After the introduction of the first trocar with a blunt tip, CO2 inflation is connected at 8 mmHg and the nipple trocar introduced until the tunnel has been created by the first trocar, under visual control.
Dissection is performed with a harmonic scalpel and following the anterior surface of the pectoralis major muscle in the clavicle direction and its insertion in the sternal notch. After this first landmark, the third trocar is introduced towards the neck.
With traction and counter-traction, dissection proceeds with the isolation of the sternocleidomastoid muscle (SCM) anterior border (second landmark) and the strap muscles anterior surface, until the middle line. Cephalad dissection ends at the thyroid cartilage (third landmark) (Figure 2).
The next step will be to isolate the lower omohyoid muscle border and set apart pre-thyroid muscle fibres. After this, the thyroid lobe is reached and its anterior surface released.
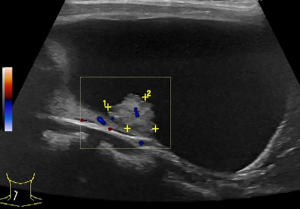
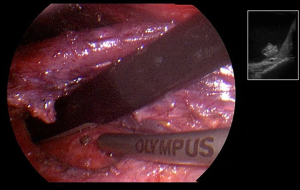
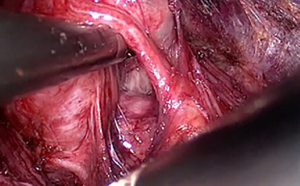
At this point, the scope is exchanged for a 5 mm laparoscope. The ultrasound probe is introduced through the 10 mm port. Complete ultrasound characterization of the cystic-solid lesion is performed with irrigation of saline to enhance image quality. A puncture with a laparoscopic needle is made under ultrasound guidance (Figures 3-5).
The reduction in size of the lobe makes life easier for the surgeon (Figure 6). Mobilization and ligation of the upper pole is the next step. Then, ligation of the middle thyroid vein, dissection of the inferior pole and identification of the recurrent laryngeal nerve are sequentially done. Afterwards, we proceed to the ligation of the inferior thyroid artery, transection of the Berry ligament and thyroid isthmus. Completed partial thyroidectomy, the specimen is removed within an endobag.
After the review of the haemostasis, the space is drained with negative pressure.
The post-operative result is very appealing (Figure 7).
The series
Three cases were approached with this technique. None was eligible for trans-axillary lobectomy according to our indications. The procedure was completed by endoscopic approach in all cases. Patients were discharged home on postoperative day one and drainage remained for an average of 4 days. No complications were recorded.
Case 1
Thirty-four-year-old female, saleswoman, no past-history of chronic diseases, referred for thyroid nodule. Ultrasound revealed a predominately cystic lesion within a lobe of 58 mm × 47 mm ×17 mm. There was an early recurrence after fine needle aspiration. No abnormal findings were noted at the biochemistry screening.
Case 2
Forty-two-year-old female, beautician, past-history of cervical spine surgery. Poor acceptance of aesthetic result of a left lateral cervical scar. Endocrine reference for complex cystic-solid lesion on the right thyroid lobe with 38 mm of maximum diameter. No alterations on contralateral lobe and no abnormal analytics.
Case 3
Thirty-nine-year-old male, airplane pilot with no history of disease and no chronic medication, who came to our department for cervical swelling. Ultrasound study reported a large thyroid right lobe with 96 mm cranium-caudal extension with a complex 74 mm × 41 mm × 50 mm lesion (cystic and solid). Left lobe with normal volume and with no lesions. Clinical biochemistry showed a normal thyroid function and no positive anti-bodies (Table 1).
Table 1
| Case | Date | Nodule size (mm3) | Lobe size (cc) | Cytology | Volume aspirated (cc) | Surgical outcome | Time of D/S (min) | Pathology |
|---|---|---|---|---|---|---|---|---|
| Case 1, F, 34 y | 03.2015 | 58×47×17 | 41.0 | Bethesda 2 | 20.0 | No complications | 6/52 | Hyperplasia |
| Case 2, F, 42 y | 07.2015 | 38×20×15 | 50.0 | Bethesda 2 | 8.0 | No complications | 5/45 | Adenoma |
| Case 3, M, 39 y | 05.2016 | 74×41×50 | 75.5 | Bethesda 1 | 30.0 | No complications | 8/62 | Follicular cyst |
Same surgeon in all cases (Jaime Vilaça). F, female; M, male; D, drainage; S, surgery.
Comments
The benefit of remote access for cervical surgery results in scarless neck surgery. Our early experience with this technique is quite exciting with low morbidity and great patient satisfaction. Their feedback encourages the team in terms of cosmetic, social, cultural and professional concerns. Our aim is to expand indications and increase safety.
To the present, our limits to perform endoscopic thyroid lobectomy are nodules not larger than 30 mm and lobes until 20 cc of volume. These clinical cases are clearly outside those indications. From a technical point of view, intra-operative volume reduction meant helping to perform a safe lobectomy.
Some East Asia surgical groups have a great experience with this technique and expanded indications greatly. To our knowledge, there are no reports on the use of a laparoscopic ultra-sound probe through an axillary port to perform intra-operative thyroid characterization and direct cystic drainage of complex lesions.
Potential benefits of trans-axillary IOUS can be:
- Intra-operative characterization of a cystic-solid lesion;
- Endoscopic surgery for large and difficult lobectomies;
- Direct puncture without risk of cytology seeding.
We also postulate that this technology can possibly aid the characterization of small isthmic nodules that need to be included in a lobectomy or the identification of parathyroid glands and their precise location. Another potential use would be to screen lymph node groups in the context of malignant disease.
Conclusions
This series reflects the experience of our group with bulky cystic-solid lesions and their trans-axillary endoscopic approach with the advent of IOUS. We believe this can be a useful tool to expand indications, facilitate the procedure and help in anatomic intraoperative recognition.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2019.03.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cohen RN, Davis AM. Management of Adult Patients With Thyroid Nodules and Differentiated Thyroid Cancer. JAMA 2017;317:434-5. [Crossref] [PubMed]
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Negro R. What happens in a 5-year follow-up of benign thyroid nodules. J Thyroid Res 2014;2014:459791. [Crossref] [PubMed]
Cite this article as: Vilaça J, Graça S, Lencastre L, Boa AF, Louro H. Trans-axillary intra-operative ultrasound cystic drainage and thyroid lobectomy: a new endoscopic approach. Ann Thyroid 2019;4:4.