
Benefits and risks of scarless thyroid surgery
Introduction
Thyroid surgery is one of the most common surgical procedures done today. In 2014, over 150,000 thyroidectomies were performed in the United States (1). Thyroidectomy traces its origins back to the Middle Ages. The first described case was the removal of a large thyroid goiter by Albucasis in present day Cordoba, Spain in 952 A.D. (2). Ancient manuscripts describe a patient sitting up in front of the surgeon with a bag around his neck to collect blood while the surgeon removed the thyroid gland through a large neck incision. As expected, this procedure had high morbidity and mortality, and because of this, fell out of favor during the Middle Ages. As noted in a review by Dr. William Halsted, the mortality rate of thyroid surgery before the 19th century was approximately 40% (2). In the late 19th century, Theodor Billroth and his pupil, Theodor Kocher drastically refined this procedure and decreased its mortality to 1% (2). Since the early 1900s, thyroid surgery has continued to evolve to be the safe procedure that it is today.
In the past four decades, the incidence of identification of thyroid nodules and the subsequent diagnosis of thyroid cancer has increased over 200% (3). Much of this is due to improved medical imaging technology and increased overall access to medical care. With approximately a 3.6% increased incidence of thyroid cancer yearly, there is now more demand for thyroid surgery (3). While thyroid cancer classically was treated with a total thyroidectomy (TT), recent guidelines suggest that treatment can be limited to thyroid lobectomy for select cases with tumors <4 cm and no evidence of metastasis or multifocality (4). In addition, active surveillance can be considered as an alternative to immediate surgery in patients with very low risk thyroid malignancies (4). These and other changes, such as encouraging patients to seek surgery at high-volume centers of excellence (5), were with the intent to decrease morbidity caused by thyroid surgery.
In efforts to further reduce morbidity, endoscopic assisted, endoscopic remote, and robotic approaches have been developed to decrease the appearance of, or even eliminate, the midline cervical scar. Minimally invasive video assisted thyroidectomy (MIVAT), described in 2005, was the first attempt at using endoscopes in order to reduce the size of the scar. This was followed by endoscopic remote-access approaches. These include, among others, the trans-axillary technique, the bilateral axillo-breast approach, and the retro-auricular (facelift) approach. While none of these approaches leave a patient with a cervical scar, each represents a surgical compromise between a remote hidden scar and extensive tissue dissection to access the thyroid (6).
Transoral endoscopic thyroidectomy vestibular approach (TOETVA) is the latest of these approaches. TOETVA was first described in the literature in 2011 by Richmon et al. (7). The first large clinical series were published by Yang in 2015 and Anuwong in 2016 featuring 41 and 60 cases conducted safely in Guangzhou, China and Bangkok, Thailand respectively (8,9). This approach uses three small incisions in the vestibule of the oral cavity to access the neck with laparoscopic ports. The surgery is performed endoscopically with the aid of carbon dioxide insufflation. Since 2016, adoption of this technique by many groups has been trialed and reported outcomes are promising. Contrary to the initial belief that this approach was only applicable to a small minority of cases, recent literature suggests that transoral endoscopic approaches to the midline neck may be widely applicable. A study published by Grogan et al. in 2019 reported that 55.8% of patients presenting to three high-volume academic centers would be adequate candidates for transoral endoscopic approach surgery (10). TOETVA is currently being performed internationally, at multiple institutions in Asia, Europe, South American, and the United States (6,11). In the following paper, we present a summary of the evidence supporting the application of this approach in select patients interested in avoiding a transcervical cutaneous scar.
Benefits of TOETVA
To date, the only well-studied benefit of TOETVA is the absence of a cutaneous scar. Although a having a midline neck scar has been historically regarded as a minor concern, it can carry significant morbidity for some patients (12,13).
Conventional open thyroidectomy leaves an appreciable transverse low cervical scar that usually ranges in size from 4–8 cm (14). The typical thyroidectomy patient is young, female (15), and more often than not, lives in a society where cosmetic concern is impressed upon its members (16). Individuals with scars, regardless of location and type are often not satisfied with their scar’s appearance and therefore adopt coping behaviors to hide the scar from perceived stigma (17). It has been well studied that patients can develop self-consciousness and psychological social stress from perceptions of the scar’s visibility (12,14,18). Visual tracking studies of open thyroidectomy patients compared to controls have shown that casual observers attend more to the neck and less to the peripheral face in patients that have a visible neck scar after open thyroid surgery (19,20). All in all, it appears these transcervical scars have some impact on quality of life (21). In fact, Choi and colleagues found that the quality of life impact associated with transcervical scars, regardless of type or severity, is similar to that found in patients with skin disorders like psoriasis and atopic dermatitis (22).
Minimally invasive approaches to thyroid removal exist and can successfully decrease the length of the transcervical scar. Nevertheless, this decreased scar length does not correlate to improved patient satisfaction (12,13,23-25). In fact, some patients are willing to undergo additional plastic surgery to improve scar appearance and cosmesis (15). Simply put, many patients do not want the traditional transcervical scar and may be willing to pay more money, travel farther and accept more medical complications just to receive a hidden scar (26,27).
In contrast to this significant quality of life impact created by a transcervical scar, TOETVA cases leave the patient with three small incisions in the oral vestibule which is a natural orifice. These mucosal incisions have been found to have a small quality of life impact (28). Many studies conducted globally with various number of TOETVA cases (4 to 81) report that all their patients have had complete postoperative satisfaction with the aesthetic appearance of their neck (8,9,29-40). Directly compared to remote access approaches like the transareolar-breast approach, TOETVA has been found to have a significantly better cosmetic effect (8,30,34,38). Furthermore, visual tracking studies have found no significant difference between TOETVA and control patients in the attention paid to their faces and necks by casual observers (19,20). This ultimately reveals that patients are getting a cosmetic result that does not distract the attention of the people around them, and thus patients are relieved of the burden of scar-induced body image distress and self-doubt. The issue is not merely a cosmetic one but one that touches on the desire for patient privacy with regards to their medical history.
In addition to significant benefits posed to the patient, to providers, TOETVA may add improved visualization of the cervical anatomy during surgery. Firstly, this approach allows excellent visualization of both recurrent laryngeal nerves (RLNs) as they insert into the larynx. Secondly, the in-plane view that is created by approaching via the oral vestibule creates a favorable angle of dissection along the plane of the recurrent laryngeal nerve. Also, the limited soft tissue dissection needed for this particular remote access technique could prove useful in patients with obesity who may have not been a candidate for other remote access approaches (6). Finally, as noted above, the broad operative indications are such that a large portion of patients presenting for thyroid surgery are candidates for this approach (10).
Rate of adoption compared to other remote access approaches
In this following section, we describe the results of our recently performed review of the global literature to compare the adoption trends of TOETVA and other remote access approaches.
Methods
Identification of the first published case series of TOETVA, trans-axillary approach thyroidectomy, bilateral axillo-breast approach thyroidectomy, and retro-auricular approach thyroidectomy was conducted. Four separate searches of the MEDLINE database were performed using the following queries: (I) “transoral endoscopic thyroidectomy vestibular approach”; (II) (“transaxillary”[tiab] OR “axillary”[tiab] OR “trans-axillary”[tiab]) AND “thyroidectomy”[tiab]; (III) (“retro-auricular”[tiab] OR “retroauricular”[tiab] OR “facelift”[tiab]) AND “thyroidectomy”[tiab]; (IV) (“Bilateral Axillo Breast approach”[tiab] OR “bilateral axillo-breast approach”[tiab] OR “BABA”[tiab]) AND “thyroidectomy”[tiab]. From the results of each query, a literature review of results was completed. Records that were not in English or published five or more years after the initial technique publication was excluded. Papers that documented cases of the technique in question were included. Cases were counted and summed cumulatively over a 5-year time period.
Results
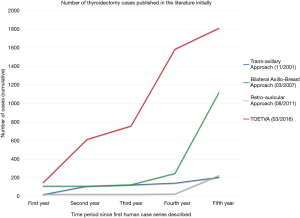
These searches of PubMed yielded 105, 283, 62, and 76 results for TOETVA, trans-axillary approach, retro-auricular approach, and BABA respectively (Figure 1). The initial case series for these four types of thyroidectomy first appeared in the literature in March 2016 (TOETVA) (9), November 2001 (trans-axillary) (41), March 2007 (BABA) (42), and August 2011 (retro-auricular) (43,44). A total of 1,813 TOETVA (6,11,29,30,34-37,40), 225 retro-auricular approach (43,45-51), 1,119 bilateral axillo-breast approach (42,52-58), and 205 trans-axillary approach (41,59-64), thyroidectomy cases were reported in the literature within the first 5 years of the technique’s existence (Table 1) (65-87). Figure 2 compares the cumulative number of cases published in the first 5 years of each approach. TOETVA had the most global range of publications in its first 5 years (16 countries) as compared to the trans-axillary (four countries), bilateral axillo-breast (one country), and retro-auricular (three countries) techniques.

Table 1
| Approach | First year | Second year | Third year | Fourth year | Fifth year | First 5 years (total) |
|---|---|---|---|---|---|---|
| Trans-axillary | 19 | 91 | 13 | 20 | 62 | 205 |
| Bilateral axillo-breast | 110 | 0 | 15 | 122 | 872 | 1,119 |
| Retro-auricular | 22 | 0 | 0 | 4 | 199 | 225 |
| TOETVA | 147 | 467 | 144 | 828 | 227 | 1,813 |
TOETVA, transoral endoscopic thyroidectomy vestibular approach.
Risks of TOETVA
In this following section, we describe the results of our recently performed review of TOETVA outcomes reported in the global literature.
Methods
A search of the MEDLINE database was conducted using the keywords “transoral endoscopic thyroidectomy vestibular approach”. Duplicate results were removed. A review of the literature describing cases performed was done. Publications that described only robotic transoral thyroidectomy cases or those that were in languages other than English were excluded. Those papers that documented at minimum the incidence of recurrent laryngeal nerve injury, hypoparathyroidism (HP), mental nerve injury (MNI), infection, conversion to open approach and operative time were included. Papers with overlapping authorship were scrutinized for cases that were reported at least once and the most inclusive publication was kept. If any questions arose about these reported cases, authors were contacted via email and clarifications were received.
Results
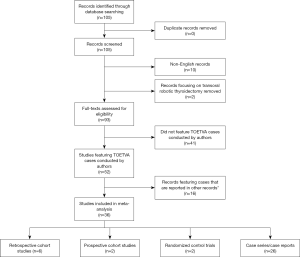
A search of PubMed yielded 105 results that were published between 2010 and May 2020. No duplicates were found. Ten titles were excluded for being in a language other than English. Two titles were excluded for describing only robotic cases. Review of the literature yielded 52 publications that met inclusion criteria. Inspection of duplicated cases narrowed this to 36 publications reporting unpublished cases. Six of these papers were retrospective cohort studies, two were prospective cohort studies, two were randomized controlled trials and 26 were case series or case reports (Figure 3).
As of May 2020, 1,880 unique TOETVA cases have been described in the literature (Table 2) (6,8,11,29,30,34-40). This represents exponential growth in the number of new cases (65-89). Of these, 571 cases (30.4%) were total thyroidectomies, 1,274 (67.8%) were lobectomies and 35 (1.9%) were isthmusectomies (Table 3). Across these 1,880 cases, the average total operation time was 124.7 minutes. In the reviewed final 36 publications, 28 TOETVA cases (approximately 1.9%) were aborted intraoperatively and converted to an open approach.
Table 2
| Authors (year) | Country (region) | Total no. of TOETVA cases | TT, n (%) | HT, n (%) | Isthmusectomy, n (%) | Average total operation time (min) | No. of conversions to open approach, n (%)** |
|---|---|---|---|---|---|---|---|
| Ahn (2020) | South Korea | 150 | 40 (26.7) | 110 (73.3) | 0 (0.0) | 110.3 | 0 (0.0) |
| Al Bisher (2020) | Saudi Arabia | 1 | 0 (0.0) | 1 (100.0) | 0 (0.0) | 270 | 0 (0.0) |
| Anuwong (2018) | Thailand | 422 | 177 (41.9) | 245 (58.1) | 0 (0.0) | 96.6 | 3 (0.7) |
| Bakkar (2018) | Jordan | 4 | 0 (0.0) | 4 (100.0) | 0 (0.0) | 122 | 1 (20.0) |
| Chai (2017) | South Korea | 10 | 0 (0.0) | 7 (70.0) | 3 (30.0) | 111.3 | 0 (0.0) |
| Chen (2018) | Taiwan | 20 | 8 (40.0) | 12 (60.0) | 0 (0.0) | 145.5 | 0 (0.0) |
| Dionigi (2017) | Italy | 15 | 5 (33.3) | 10 (66.7) | 0 (0.0) | 96.3 | 0 (0.0) |
| Fernandez Ranvier (2020) | USA, Spain, Switzerland, Taiwan | 152* | 38 (25.0) | 114 (75.0) | 0 (0.0) | 174.2 | 3 (2.0) |
| Fu (2018) | China | 81* | 10 (12.4) | 65 (80.3) | 6 (0.1) | 89 | 2 (2.4) |
| Guo (2020) | China | 40 | 0 (0.0) | 40 (100.0) | 0 (0.0) | 172 | 0 (0.0) |
| Jitpratoom (2016) | Thailand | 45 | 45 (100.0) | 0 (0.0) | 0 (0.0) | 134.1 | 1 (2.2) |
| Kadem (2019) | Iraq | 10 | 1 (10.0) | 9 (90.0) | 0 (0.0) | 113.5 | 0 (0.0) |
| Kim (2020) | South Korea | 132 | 8 (6.06) | 110 (83.3) | 14 (10.6) | 87.6 | 0 (0.0) |
| Le (2018) | Vietnam | 1 | 1 (100.0) | 0 (0.0) | 0 (0.0) | 110 | 0 (0.0) |
| Le (2020) | Vietnam | 28 | 0 (0.0) | 28 (100.0) | 0 (0.0) | 91 | 0 (0.0) |
| Luna-Ortiz (2020) | Mexico | 46* | 44 (95.7) | 2 (4.4) | 0 (0.0) | 207 | 6 (13.0) |
| Luo (2020) | China | 204 | 52 (25.5) | 152 (74.5) | 0 (0.0) | 147.99 | 2 (1.0) |
| Nakajo (2013) | Japan | 8 | 3 (37.5) | 5 (62.5) | 0 (0.0) | 265.38 | 0 (0.0) |
| Park (2019) | South Korea | 65 | 10 (15.4) | 55 (84.6) | 0 (0.0) | 147.5 | 0 (0.0) |
| Park (2019) | South Korea | 15 | 2 (13.3) | 12 (80.0) | 1 (6.7) | 138.67 | 0 (0.0) |
| Park (2020) | South Korea | 1 | 0 (0.0) | 0 (0.0) | 1 (100.0) | 98.7 | 0 (0.0) |
| Pérez-Soto (2019) | Mexico | 20* | 17 (85.0) | 3 (15.0) | 0 (0.0) | 216.7 | 3 (15.0) |
| Russell (2019) | USA | 92* | 0 (0.0) | 92 (100.0) | 0 (0.0) | 126.00 | 1 (1.1) |
| Sivakumar (2018) | India | 11 | 11 (100.0) | 0 (0.0) | 0 (0.0) | 130 | 0 (0.0) |
| Tan (2019) | China | 20 | 20 (100.0) | 0 (0.0) | 0 (0.0) | 145.95 | 0 (0.0) |
| Tesseroli (2018) | Brazil | 9 | 8 (88.9) | 1 (11.1) | 0 (0.0) | 196.1 | 0 (0.0) |
| Udelsman (2016) | USA | 5 | 2 (40.0) | 3 (60.0) | 0 (0.0) | 244.8 | 0 (0.0) |
| Wang (2014) | China | 12 | 4 (33.3) | 8 (66.7) | 0 (0.0) | 60.4 | 0 (0.0) |
| Wilhelm (2016) | Germany, China | 93 | 17 (18.3) | 66 (71.0) | 10 (10.8) | 109.78 | 3 (3.1) |
| Wu (2018) | Taiwan | 27 | 18 (66.7) | 9 (33.3) | 0 (0.0) | 259.33 | 0 (0.0) |
| Xu (2019) | China | 48 | 0 (0.0) | 48 (100.0) | 0 (0.0) | 107.2 | 0 (0.0) |
| Yang (2015) | China | 41 | 22 (53.7) | 19 (46.3) | 0 (0.0) | 72.1 | 0 (0.0) |
| Yang (2016) | China | 6 | 0 (0.0) | 6 (100.0) | 0 (0.0) | 122 | 0 (0.0) |
| Zeng (2016) | China | 4 | 0 (0.0) | 4 (100.0) | 0 (0.0) | 189 | 0 (0.0) |
| Zhang (2018) | Italy | 1 | 1 (100.0) | 0 (0.0) | 0 (0.0) | 110 | 0 (0.0) |
| Zhang (2019) | Italy | 41 | 7 (17.1) | 34 (82.9) | 0 (0.0) | 109 | 3 (6.8) |
*, This number includes the converted cases; **, out of total TOETVA cases attempted. TOETVA, transoral endoscopic thyroidectomy vestibular approach; TT, total thyroidectomy; HT, hemithyroidectomy.
Table 3
| Total no. of TOETVA cases | TT, n (%) | HT, n (%) | Isthmusectomy, n (%) | Average total operation time (min) | No. of conversions to open approach, n (%)** |
|---|---|---|---|---|---|
| 1,880* | 571 (30.4) | 1,274 (67.8) | 35 (1.9) | 124.7 | 28 (1.8) |
*, This number includes some of the converted cases; **, out of total TOETVA cases attempted. TOETVA, transoral endoscopic thyroidectomy vestibular approach; TT, total thyroidectomy; HT, hemithyroidectomy.
An assessment of reported complications from these cases was conducted (Table 4). Carbon dioxide embolism occurred in 5 cases (0.3%). Hematoma occurred in 8 cases (0.4%), and surgical site infection in 20 cases (1.1%) (Table 5). With regards to injury of the recurrent laryngeal nerve, transient RLN palsy was observed in 74 cases (3.9%) and permanent RLN palsy noted in 11 (0.6%). HP was mentioned as a complication in some cases, occurring transiently in 96 (16.8%) and permanently in 5 cases (0.9%). MNI, defined by lower lip or chin paresthesia (90), was noted transiently in 113 cases (6%) and permanently in 2 cases (0.1%).
Table 4
| Authors (year) | Hematoma, n (%) | Transient RLN palsy, n (%) | Permanent RLN palsy, n (%) | Transient HP, n (%)** | Permanent HP, n (%)** | Transient MNI, n (%) | Permanent MNI, n (%) | Infection, n (%) | CO2 embolism, n (%) |
|---|---|---|---|---|---|---|---|---|---|
| Ahn (2020) | 1 (0.7) | 7 (4.7) | 1 (0.7) | 5 (12.5) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Al Bisher (2020) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Anuwong (2018) | 1 (0.2) | 25 (5.9) | 0 (0.0) | 46 (26.0) | 0 (0.0) | 3 (0.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Bakkar (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Chai (2017) | 0 (0.0) | 2 (20.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 1 (10.0) | 0 (0.0) |
| Chen (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 3 (37.5) | 0 (0.0) | 1 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Dionigi (2017) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Fernandez Ranvier (2020) | 3 (2.0)* | 5 (3.3)* | 3 (2.0)* | 7 (18.4)* | 0 (0.0) | 62 (40.8)* | 1 (0.7)* | 1 (0.7)* | 0 (0.0) |
| Fu (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 6 (7.4)* | 2 (2.4)* |
| Guo (2020) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 1 (2.5) | 0 (0.0) |
| Jitpratoom (2016) | 0 (0.0) | 4 (8.9) | 0 (0.0) | 10 (22.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Kadem (2019) | 0 (0.0) | 1 (10.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Kim (2020) | 1 (0.8) | 6 (4.6) | 0 (0.0) | 1 (12.5) | 0 (0.0) | 2 (1.5) | 1 (0.8) | 1 (0.8) | 0 (0.0) |
| Le (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Le (2020) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 1 (3.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Luna-Ortiz (2020) | 0 (0.0) | 1 (2.2)* | 2 (4.4)* | 0 (0.0) | 2 (4.6)* | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Luo (2020) | 0 (0.0) | 6 (2.9) | 2 (1.0) | 10 (19.2) | 1 (1.9) | 1 (0.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Nakajo (2013) | 0 (0.0) | 0 (0.0) | 1 (12.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Park (2019) | 0 (0.0) | 2 (3.1) | 1 (1.5) | 5 (50) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Park (2019) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (50) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Park (2020) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Pérez-Soto (2019) | 1 (5.0)* | 2 (10.0)* | 0 (0.0) | 5 (29.4)* | 0 (0.0) | 3 (15.0)* | 0 (0.0) | 1 (5.0)* | 0 (0.0) |
| Russell (2019) | 0 (0.0) | 4 (4.4) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sivakumar (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Tan (2019) | 0 (0.0) | 1 (5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Tesseroli (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Udelsman (2016) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Wang (2014) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Wilhelm (2016) | 0 (0.0) | 1 (1.1) | 1 (1.1) | 0 (0.0) | 0 (0.0) | 15 (16.1) | 0 (0.0) | 6 (6.5) | 3 (3.2) |
| Wu (2018) | 0 (0.0) | 4 (14.8) | 0 (0.0) | 1 (5.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 1 (3.7) | 0 (0.0) |
| Xu (2019) | 1 (2.1) | 1 (2.1) | 0 (0.0) | – | – | 22 (45.8) | 0 (0.0) | 1 (2.1) | 0 (0.0) |
| Yang (2015) | 0 (0.0) | 1 (2.4) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Yang (2016) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 1 (16.7) | 0 (0.0) |
| Zeng (2016) | 0 (0.0) | 0 (0.0) | 0 (0.0) | – | – | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Zhang (2018) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Zhang (2019) | 0 (0.0) | 1 (2.4) | 0 (0.0) | 1 (14.3) | 0 (0.0) | 3 (7.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
*, Out of the total TOETVA cases attempted rather than completed. See Table 1; **, out of TT cases. TOETVA, transoral endoscopic thyroidectomy vestibular approach; TT, total thyroidectomy; RLN, recurrent laryngeal nerve; HP, hypoparathyroidism; MNI, mental nerve injury.
Table 5
| Hematoma, n (%) | Transient RLN palsy, n (%) | Permanent RLN palsy, n (%) | Transient HP, n (%)* | Permanent HP, n (%)* | Transient MNI, n (%) | Permanent MNI, n (%) | Infection, n (%) | CO2 embolism, n (%) |
|---|---|---|---|---|---|---|---|---|
| 8 (0.4) | 74 (3.9) | 11 (0.6) | 96 (16.8) | 5 (0.9) | 113 (6) | 2 (0.1) | 20 (1.1) | 5 (0.2) |
*, Out of TT cases. TT, total thyroidectomy; TOETVA, transoral endoscopic thyroidectomy vestibular approach; RLN, recurrent laryngeal nerve; HP, hypoparathyroidism; MNI, mental nerve injury.
Discussion
This review of TOETVA in the global literature establishes that TOETVA is increasingly common, has a safety profile similar to that of standard open thyroidectomy techniques (91-93), and reduces significant patient morbidity related to the transcervical scar.
TOETVA is feasible for both benign and malignant indications and this approach can be used for isthmusectomy, thyroid lobectomy and TT with or without central neck dissection. Although total operation time largely depends on the logistics of the operating environment and the experience of the surgeon, the average total operating time approximates 2 hours. This further supports the belief that the duration is similar to that of an open thyroidectomy (94). Additionally, intraoperative conversion to an open approach is rare (1.9%). Postoperative complications such as hematoma, infection, HP, and recurrent laryngeal nerve dysfunction are observed in patients undergoing all types of thyroidectomy. The outcomes after TOETVA are similar to those seen after open thyroidectomy (91-93). At a minimum, the safety of TOETVA does not appear to be inferior to the classic open thyroidectomy approach.
TOETVA introduces new complications that are not typically observed in the conventional approach such as risk of carbon dioxide embolism and MNI. Our review suggests that carbon dioxide embolism rarely occurs. MNI, defined as paresthesia of the lower lip or chin region, was the most common complication in the cases reported. Almost all of these complications were self-limited, with only permanent MNI seen in two cases. Similar hypoesthesia is often created anywhere flap elevation is completed, and generally recovers over time.
This review is not without limitations. Most significantly, we acknowledge that there are complications that have been underreported or not reported at all. Complications such as carbon dioxide embolus were reported more frequently in the past but have not been described in the literature for several years. While this could represent an evolution in the safety of the approach, it could also represent a publication bias. Despite these concerns, however, it is apparent that TOETVA is being widely adopted globally (Table 6), and these studies represent the combined results of those institutions with the largest volumes to date.
Table 6
| Country | Publications | Total TOETVA cases | TT cases, n (%) | Total HT cases, n (%) | Total isthmusectomy cases, n (%) |
|---|---|---|---|---|---|
| Brazil | Tesseroli (2018) | 9 | 8 | 1 | 0 |
| China | Fu (2018), Guo (2020), Luo (2020), Tan (2019), Wang (2014), Wilhelm (2016), Xu (2019), Yang (2015), Yang (2016), Zeng (2016) | 549** | 125 (22.8)** | 408 (74.3)** | 16 (0.3)** |
| Germany | Wilhelm (2016) | 93** | 17 (18.2)** | 66 (71)** | 10 (10.8)** |
| India | Sivakumar (2018) | 11 | 11 (100.0) | 0 (0.0) | 0 (0.0) |
| Iraq | Kadem (2019) | 10 | 1 (10.0) | 9 (90.0) | 0 (0.0) |
| Italy | Dionigi (2017), Zhang (2018), Zhang (2019) | 57 | 13 (22.8) | 44 (77.2) | 0 (0.0) |
| Japan | Nakajo (2013) | 8 | 3 (37.5) | 5 (62.5) | 0 (0.0) |
| Jordan | Bakkar (2018) | 4 | 0 (0.0) | 4 (100.0) | 0 (0.0) |
| Mexico | Luna-Ortiz (2020), Pérez-Soto (2019) | 66 | 61 (92.4) | 5 (7.6) | 0 (0.0) |
| Saudi Arabia | Al Bisher (2020) | 1 | 0 (0.0) | 1 (100.0) | 0 (0.0) |
| South Korea | Ahn (2020), Chai (2017), Kim (2020), Park (2019), Park (2019), Park (2020) | 373 | 60 (16.1) | 294 (78.8) | 19 (5.1) |
| Spain | Fernandez Ranvier (2020) | 29* | 6 (20.7)* | 23 (79.3)* | 0 (0.0) |
| Switzerland | Fernandez Ranvier (2020) | 29* | 6 (20.7)* | 23 (79.3)* | 0 (0.0) |
| Taiwan | Chen (2018), Fernandez Ranvier (2020), Wu (2018) | 88 | 36 (40.9) | 52 (59.1) | 0 (0.0) |
| Thailand | Anuwong (2018), Jitpratoom (2016) | 467 | 222 (47.5) | 245 (52.5) | 0 (0.0) |
| USA | Fernandez Ranvier (2020), Russell (2019), Udelsman (2016) | 179 | 24 (13.4) | 155 (86.6) | 0 (0.0) |
| Vietnam | Le (2018), Le (2020) | 29 | 1 (3.4) | 28 (96.6) | 0 (0.0) |
*, Fernandez Ranvier et al. (2020) reports Spanish and Swiss cases together; **, Wilhelm et al. (2016) includes cases from both China and Germany. TOETVA, transoral endoscopic thyroidectomy vestibular approach; TT, total thyroidectomy; HT, hemithyroidectomy.
While it remains to be seen whether TOETVA becomes a standard alternative to open thyroidectomy, interest in the technique is growing. Our review of the first 5 years of published remote access approach cases in the literature establishes that, at least in the academic thyroid surgery community, TOETVA has been embraced more rapidly than the trans-axillary, bilateral axillo-breast and retro-auricular approaches in their initial years (Figure 2).
Lastly, the COVID-19 pandemic caused by widespread SARS-CoV-2 virus infection around the globe has led us to reevaluate our management of surgical candidates. It is important to proceed with caution while minimizing risk to patients and healthcare workers. At this point we would recommend SARS-CoV-2 testing of all TOETVA candidates and use of adequate personal protective equipment during this and other thyroidectomy approaches. We should consider the possibility of increased aerosolization during this approach when compared to conventional approaches.
Conclusions
TOETVA has been widely adopted across the globe and should be considered a novel but safe approach to thyroid surgery. It provides excellent cosmesis while demonstrating non-inferiority in terms of risk to the patient (RLN palsy, bleeding, infection, HP). Larger prospective studies should be done in the future to compare TOETVA to traditional thyroidectomy in terms of quality of life, voice outcomes and oncologic equivalency.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marcin Barczyński and Maurizio Iacobone) for the series “Recent Challenges in the Management of Thyroid Tumors” published in Annals of Thyroid. The article has undergone external peer review.
Peer Review File: Available at http://dx.doi.org/10.21037/aot-20-52
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot-20-52). The series “Recent Challenges in the Management of Thyroid Tumors” was commissioned by the editorial office without any funding or sponsorship. Dr. JOR reports personal fees from Baxter, outside the submitted work. Dr. RPT reports personal fees from Medtronic, personal fees from Hemostatix, personal fees from RGS Healthcare, outside the submitted work. The other authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Francis DO, Randolph G, Davies L. Nationwide variation in rates of thyroidectomy among us medicare beneficiaries. JAMA Otolaryngol Head Neck Surg 2017;143:1122-5. [Crossref] [PubMed]
- Sarkar S, Banerjee S, Sarkar R, et al. A review on the history of 'thyroid surgery'. Indian J Surg 2016;78:32-6. [Crossref] [PubMed]
- Lim H, Devesa SS, Sosa JA, et al. Trends in thyroid cancer incidence and mortality in the United States, 1974-2013. JAMA 2017;317:1338-48. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines Task Force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Meltzer C, Klau M, Gurushanthaiah D, et al. Surgeon volume in thyroid surgery: Surgical efficiency, outcomes, and utilization. Laryngoscope 2016;126:2630-9. [Crossref] [PubMed]
- Fernandez Ranvier G, Meknat A, Guevara DE, et al. International multi-institutional experience with the transoral endoscopic thyroidectomy vestibular approach. J Laparoendosc Adv Surg Tech A 2020;30:278-83. [Crossref] [PubMed]
- Richmon JD, Pattani KM, Benhidjeb T, et al. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck 2011;33:330-3. [PubMed]
- Yang J, Wang C, Li J, et al. Complete endoscopic thyroidectomy via oral vestibular approach versus areola approach for treatment of thyroid diseases. J Laparoendosc Adv Surg Tech A 2015;25:470-6. [Crossref] [PubMed]
- Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Grogan RH, Suh I, Chomsky-Higgins K, et al. Patient eligibility for transoral endocrine surgery procedures in the United States. JAMA Netw Open 2019;2:e194829. [Crossref] [PubMed]
- Tesseroli MAS, Spagnol M, Sanabria Á. Transoral endoscopic thyroidectomy by vestibular approach (TOETVA): initial experience in Brazil. Rev Col Bras Cir 2018;45:e1951. [Crossref] [PubMed]
- Sethukumar P, Ly D, Awad Z, et al. Scar satisfaction and body image in thyroidectomy patients: prospective study in a tertiary referral centre. J Laryngol Otol 2018;132:60-7. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: a prospective cohort study. Int J Surg 2016;25:38-43. [Crossref] [PubMed]
- Koo DH, Kim DM, Choi JY, et al. In-depth survey of scarring and distress in patients undergoing bilateral axillo-breast approach robotic thyroidectomy or conventional open thyroidectomy. Surg Laparosc Endosc Percutan Tech 2015;25:436-9. [Crossref] [PubMed]
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Dionigi G, Lavazza M, Wu CW, et al. Transoral thyroidectomy: why is it needed? Gland Surg 2017;6:272-6. [Crossref] [PubMed]
- Brown BC, McKenna SP, Siddhi K, et al. The hidden cost of skin scars: quality of life after skin scarring. J Plast Reconstr Aesthet Surg 2008;61:1049-58. [Crossref] [PubMed]
- Babin E, Sigston E, Hitier M, et al. Quality of life in head and neck cancers patients: predictive factors, functional and psychosocial outcome. Eur Arch Otorhinolaryngol 2008;265:265-70. [Crossref] [PubMed]
- Liao D, Ishii LE, Chen LW, et al. Transoral neck surgery prevents attentional bias towards the neck compared to open neck surgery. Laryngoscope 2020;130:1603-8. [Crossref] [PubMed]
- Juarez MC, Ishii L, Nellis JC, et al. Objectively measuring social attention of thyroid neck scars and transoral surgery using eye tracking. Laryngoscope 2019;129:2789-94. [Crossref] [PubMed]
- Balci DD, Inandi T, Dogramaci CA, et al. DLQI scores in patients with keloids and hypertrophic scars: a prospective case control study. J Dtsch Dermatol Ges 2009;7:688-92. [Crossref] [PubMed]
- Choi Y, Lee JH, Kim YH, et al. Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients. Ann Dermatol 2014;26:693-9. [Crossref] [PubMed]
- Kim SM, Chun KW, Chang HJ, et al. Reducing neck incision length during thyroid surgery does not improve satisfaction in patients. Eur Arch Otorhinolaryngol 2015;272:2433-8. [Crossref] [PubMed]
- Toll EC, Loizou P, Davis CR, et al. Scars and satisfaction: do smaller scars improve patient-reported outcome? Eur Arch Otorhinolaryngol 2012;269:309-13. [Crossref] [PubMed]
- Linos D, Economopoulos KP, Kiriakopoulos A, et al. Scar perceptions after thyroid and parathyroid surgery: comparison of minimal and conventional approaches. Surgery 2013;153:400-7. [Crossref] [PubMed]
- Sukpanich R, Sanglestsawai S, Seib CD, et al. The influence of cosmetic concerns on patient preferences for approaches to thyroid lobectomy: a discrete choice experiment. Thyroid 2020;30:1306-13. [Crossref] [PubMed]
- Coorough NE, Schneider DF, Rosen MW, et al. A survey of preferences regarding surgical approach to thyroid surgery. World J Surg 2014;38:696-703. [Crossref] [PubMed]
- Russell JO, Clark J, Noureldine SI, et al. Transoral thyroidectomy and parathyroidectomy - A North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol 2017;71:75-80. [Crossref] [PubMed]
- Le QV, Ngo DQ, Tran TD, et al. Transoral endoscopic thyroidectomy vestibular approach: an initial experience in Vietnam. Surg Laparosc Endosc Percutan Tech 2020;30:209-13. [Crossref] [PubMed]
- Xu Z, Song J, Wang Y, et al. A comparison of transoral vestibular and bilateral areolar endoscopic thyroidectomy approaches for unilateral papillary thyroid microcarcinomas. Wideochir Inne Tech Maloinwazyjne 2019;14:501-8. [Crossref] [PubMed]
- Wang Y, Zhang Z, Zhao Q, et al. Transoral endoscopic thyroid surgery via the tri-vestibular approach with a hybrid space-maintaining method: a preliminary report. Head Neck 2018;40:1774-9. [Crossref] [PubMed]
- Yi JW, Yoon SG, Kim HS, et al. Transoral endoscopic surgery for papillary thyroid carcinoma: initial experiences of a single surgeon in South Korea. Ann Surg Treat Res 2018;95:73-9. [Crossref] [PubMed]
- Wang T, Wu Y, Xie Q, et al. Safety of central compartment neck dissection for transoral endoscopic thyroid surgery in papillary thyroid carcinoma. Jpn J Clin Oncol 2020;50:387-91. [Crossref] [PubMed]
- Guo F, Wang W, Zhu X, et al. Comparative study between endoscopic thyroid surgery via the oral vestibular approach and the areola approach. J Laparoendosc Adv Surg Tech A 2020;30:170-4. [Crossref] [PubMed]
- Tan Y, Guo B, Deng X, et al. Transoral endoscopic selective lateral neck dissection for papillary thyroid carcinoma: a pilot study. Surg Endosc 2020;34:5274-82. [Crossref] [PubMed]
- Dionigi G, Bacuzzi A, Lavazza M, et al. Transoral endoscopic thyroidectomy: preliminary experience in Italy. Updates Surg 2017;69:225-34. [Crossref] [PubMed]
- Fu J, Luo Y, Chen Q, et al. Transoral endoscopic thyroidectomy: review of 81 cases in a single institute. J Laparoendosc Adv Surg Tech A 2018;28:286-91. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Yang K, Ding B, Lin C, et al. The novel transvestibule approach for endoscopic thyroidectomy: a case series. Surg Laparosc Endosc Percutan Tech 2016;26:e25-8. [Crossref] [PubMed]
- Zeng YK, Li ZY, Xuan WL, et al. Trans-oral glasses-free three-dimensional endoscopic thyroidectomy-preliminary single center experiences. Gland Surg 2016;5:628-32. [Crossref] [PubMed]
- Ikeda Y, Takami H, Niimi M, et al. Endoscopic thyroidectomy and parathyroidectomy by the axillary approach. A preliminary report. Surg Endosc 2002;16:92-5. [Crossref] [PubMed]
- Choe JH, Kim SW, Chung KW, et al. Endoscopic thyroidectomy using a new bilateral axillo-breast approach. World J Surg 2007;31:601-6. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: patient selection and technical considerations. Surg Laparosc Endosc Percutan Tech 2011;21:237-42. [Crossref] [PubMed]
- Berber E, Bernet V, Fahey TJ 3rd, et al. American thyroid association statement on remote-access thyroid surgery. Thyroid 2016;26:331-7. [Crossref] [PubMed]
- Terris DJ, Singer MC. Robotic facelift thyroidectomy: Facilitating remote access surgery. Head Neck 2012;34:746-7. [Crossref] [PubMed]
- Kandil E, Saeed A, Mohamed SE, et al. Modified robotic-assisted thyroidectomy: an initial experience with the retroauricular approach. Laryngoscope 2015;125:767-71. [Crossref] [PubMed]
- Chung EJ, Park MW, Cho JG, et al. A prospective 1-year comparative study of endoscopic thyroidectomy via a retroauricular approach versus conventional open thyroidectomy at a single institution. Ann Surg Oncol 2015;22:3014-21. [Crossref] [PubMed]
- Lee DY, Lee KJ, Han WG, et al. Comparison of transaxillary approach, retroauricular approach, and conventional open hemithyroidectomy: a prospective study at single institution. Surgery 2016;159:524-31. [Crossref] [PubMed]
- Byeon HK. Comprehensive application of robotic retroauricular thyroidectomy: the evolution of robotic thyroidectomy. Laryngoscope 2016;126:1952-7. [Crossref] [PubMed]
- Lira RB, Chulam TC, Koh YW, et al. Retroauricular endoscope-assisted approach to the neck: early experience in Latin America. Int Arch Otorhinolaryngol 2016;20:138-44. [Crossref] [PubMed]
- Sung ES, Ji YB, Song CM, et al. Robotic thyroidectomy: comparison of a postauricular facelift approach with a gasless unilateral axillary approach. Otolaryngol Head Neck Surg 2016;154:997-1004. [Crossref] [PubMed]
- Lee KE, Rao J, Youn YK. Endoscopic thyroidectomy with the da Vinci robot system using the bilateral axillary breast approach (BABA) technique: our initial experience. Surg Laparosc Endosc Percutan Tech 2009;19:e71-5. [Crossref] [PubMed]
- Kim SJ, Lee KE, Choe JH, et al. Endoscopic completion thyroidectomy by the bilateral axillo-breast approach. Surg Laparosc Endosc Percutan Tech 2010;20:312-6. [Crossref] [PubMed]
- Lee KE. Outcomes of 109 patients with papillary thyroid carcinoma who underwent robotic total thyroidectomy with central node dissection via the bilateral axillo-breast approach. Surgery 2010;148:1207-13. [Crossref] [PubMed]
- Lee KE, Choi JY, Youn YK. Bilateral axillo-breast approach robotic thyroidectomy. Surg Laparosc Endosc Percutan Tech 2011;21:230-6. [Crossref] [PubMed]
- Hur SM, Kim SH, Lee SK, et al. New endoscopic thyroidectomy with the bilateral areolar approach: a comparison with the bilateral axillo-breast approach. Surg Laparosc Endosc Percutan Tech 2011;21:e219-24. [Crossref] [PubMed]
- Im HJ. Evaluation of surgical completeness in endoscopic thyroidectomy compared with open thyroidectomy with regard to remnant ablation. Clin Nucl Med 2012;37:148-51. [Crossref] [PubMed]
- Kim HY, d'Ajello F, Woo SU, et al. Robotic thyroid surgery using bilateral axillo-breast approach: personal initial experience over two years. Minerva Chir 2012;67:39-48. [PubMed]
- Ikeda Y, Takami H, Sasaki Y, et al. Clinical benefits in endoscopic thyroidectomy by the axillary approach. J Am Coll Surg 2003;196:189-95. [Crossref] [PubMed]
- Chantawibul S, Lokechareonlarp S, Pokawatana C. Total video endoscopic thyroidectomy by an axillary approach. J Laparoendosc Adv Surg Tech A 2003;13:295-9. [Crossref] [PubMed]
- Udomsawaengsup S, Navicharern P, Tharavej C, et al. Endoscopic transaxillary thyroid lobectomy: flexible vs rigid laparoscope. J Med Assoc Thai 2004;87:S10-4. [PubMed]
- Ikeda Y, Takami H, Sasaki Y, et al. Are there significant benefits of minimally invasive endoscopic thyroidectomy? World J Surg 2004;28:1075-8. [Crossref] [PubMed]
- Duncan TD, Ejeh IA, Speights F, et al. Endoscopic transaxillary near total thyroidectomy. JSLS 2006;10:206-11. [PubMed]
- Yoon JH, Park CH, Chung WY. Gasless endoscopic thyroidectomy via an axillary approach: experience of 30 cases. Surg Laparosc Endosc Percutan Tech 2006;16:226-31. [Crossref] [PubMed]
- Al Bisher HM, Khidr AM, Alkhudair BH, et al. Transoral endoscopic thyroidectomy via vestibular approach: first case in Saudi Arabia. Int J Surg Case Rep 2020;70:75-7. [Crossref] [PubMed]
- Ahn JH, Yi JW. Transoral endoscopic thyroidectomy for thyroid carcinoma: outcomes and surgical completeness in 150 single-surgeon cases. Surg Endosc 2020;34:861-7. [Crossref] [PubMed]
- Anuwong A, Ketwong K, Jitpratoom P, et al. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg 2018;153:21-7. [Crossref] [PubMed]
- Chai YJ, Chung JK, Anuwong A, et al. Transoral endoscopic thyroidectomy for papillary thyroid microcarcinoma: initial experience of a single surgeon. Ann Surg Treat Res 2017;93:70-5. [Crossref] [PubMed]
- Chen HK, Chen CL, Wen KS, et al. Application of transoral continuous intraoperative neuromonitoring in natural orifice transluminal endoscopic surgery for thyroid disease: a preliminary study. Surg Endosc 2018;32:517-25. [Crossref] [PubMed]
- Bakkar S, Al Hyari M, Naghawi M, et al. Transoral thyroidectomy: a viable surgical option with unprecedented complications-a case series. J Endocrinol Invest 2018;41:809-13. [Crossref] [PubMed]
- Jitpratoom P, Ketwong K, Sasanakietkul T, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves' disease: a comparison of surgical results with open thyroidectomy. Gland Surg 2016;5:546-52. [Crossref] [PubMed]
- Kadem SG, Habash SM, Jasim AH. Transoral endoscopic thyroidectomy via vestibular approach: a series of the first ten cases in Iraq. Sultan Qaboos Univ Med J 2019;19:e68-72. [Crossref] [PubMed]
- Kim SY, Kim SM, Makay Ö, et al. Transoral endoscopic thyroidectomy using the vestibular approach with an endoscopic retractor in thyroid cancer: experience with the first 132 patients. Surg Endosc 2020;34:5414-20. [Crossref] [PubMed]
- Le QV, Ngo DQ, Ngo QX. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): a case report as new technique in thyroid surgery in Vietnam. Int J Surg Case Rep 2018;50:60-3. [Crossref] [PubMed]
- Park JH, Bilegsaikhan SE, Suh YJ. A Novel technique for performing transoral endoscopic thyroidectomy vestibular approach (TOETVA): a single-port platform. Surg Laparosc Endosc Percutan Tech 2020;30:e4-7. [Crossref] [PubMed]
- Luna-Ortiz K, Gómez-Pedraza A, Anuwong A. Lessons learned from the transoral endoscopic thyroidectomy with vestibular approach (TOETVA) for the treatment of thyroid carcinoma. Ann Surg Oncol 2020;27:1356-60. [Crossref] [PubMed]
- Luo JH, Xiang C, Wang P, et al. The learning curve for transoral endoscopic thyroid surgery: a single surgeon's 204 case experience. J Laparoendosc Adv Surg Tech A 2020;30:163-9. [Crossref] [PubMed]
- Park JO, Anuwong A, Kim MR, et al. Transoral endoscopic thyroid surgery in a Korean population. Surg Endosc 2019;33:2104-13. [Crossref] [PubMed]
- Park JO, Park YJ, Kim MR, et al. Gasless transoral endoscopic thyroidectomy vestibular approach (gasless TOETVA). Surg Endosc 2019;33:3034-9. [Crossref] [PubMed]
- Pérez-Soto RH, Ponce de León-Ballesteros G, Montalvo-Hernández J, et al. Transoral endoscopic thyroidectomy by vestibular approach-initial experience and comparative analysis in the first reported mexican cohort. J Laparoendosc Adv Surg Tech A 2019;29:1526-31. [Crossref] [PubMed]
- Russell JO, Razavi CR, Garstka ME, et al. Remote-access thyroidectomy: a multi-institutional North American experience with transaxillary, robotic facelift, and transoral endoscopic vestibular approaches. J Am Coll Surg 2019;228:516-22. [Crossref] [PubMed]
- Sivakumar T, Amizhthu RA. Transoral endoscopic total thyroidectomy vestibular approach: a case series and literature review. J Minim Access Surg 2018;14:118-23. [Crossref] [PubMed]
- Udelsman R, Anuwong A, Oprea AD, et al. Trans-oral vestibular endocrine surgery: a new technique in the United States. Ann Surg 2016;264:e13-6. [Crossref] [PubMed]
- Wilhelm T, Wu G, Teymoortash A, et al. Transoral endoscopic thyroidectomy: current state of the art—a systematic literature review and results of a bi-center study. Transl Cancer Res 2016;5:S1521-30. [Crossref]
- Wu YJ, Chi SY, Elsarawy A, et al. What is the appropriate nodular diameter in thyroid cancer for extraction by transoral endoscopic thyroidectomy vestibular approach without breaking the specimens? A surgicopathologic study. Surg Laparosc Endosc Percutan Tech 2018;28:390-3. [Crossref] [PubMed]
- Zhang D, Caruso E, Sun H, et al. Classifying pain in transoral endoscopic thyroidectomy. J Endocrinol Invest 2019;42:1345-51. [Crossref] [PubMed]
- Zhang D, Wu CW, Inversini D, et al. Lessons learned from a faulty transoral endoscopic thyroidectomy vestibular approach. Surg Laparosc Endosc Percutan Tech 2018;28:e94-9. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Russell JO, Razavi CR, Shaear M, et al. Transoral vestibular thyroidectomy: current state of affairs and considerations for the future. J Clin Endocrinol Metab 2019;104:3779-84. [Crossref] [PubMed]
- Nguyen J, Duong H. Anatomy, Head and Neck, Mental Nerve. In: StatPearls. Treasure Island: StatPearls Publishing, 2020.
- Bhattacharyya N, Fried MP. Assessment of the morbidity and complications of total thyroidectomy. Arch Otolaryngol Head Neck Surg 2002;128:389-92. [Crossref] [PubMed]
- Meltzer C, Hull M, Sundang A, et al. Association between annual surgeon total thyroidectomy volume and transient and permanent complications. JAMA Otolaryngol Head Neck Surg 2019;145:830-7. [Crossref] [PubMed]
- Lee M, Rhee J, Kim Y, et al. Perioperative risk factors for post-thyroidectomy hematoma: Significance of pain and ketorolac usage. Head Neck 2019;41:3656-60. [Crossref] [PubMed]
- Patoir A, Payet C, Peix JL, et al. Determinants of operative time in thyroid surgery: A prospective multicenter study of 3454 thyroidectomies. PLoS One 2017;12:e0181424. [Crossref] [PubMed]
Cite this article as: Banuchi VE, Ballakur SS, Russell JO, Tufano RP. Benefits and risks of scarless thyroid surgery. Ann Thyroid 2020;5:24.


