
Thyroid isthmusectomy for a benign nodule of the thyroid isthmus, a case report
Introduction
Current surgical guidelines for a solitary, cytologically indeterminate nodule, recommend a thyroid lobectomy (1). There are currently no guidelines that discuss the surgical management of nodules isolated to the pyramidal lobe or thyroid isthmus. The significant complications associated with a thyroid lobectomy includes damage to the parathyroid glands or superior and recurrent laryngeal nerves. The documented incidence of these complications is 1.9% for a parathyroid injury and up to 14% for laryngeal nerve injury with a unilateral thyroid lobectomy (2,3). A thyroid isthmusectomy lowers the risk of these complications, as there is no anatomical exposure to the superior or recurrent laryngeal nerves. The presence of a parathyroid gland on the trachea, inferior to the isthmus is extremely low. An isolated thyroid isthmusectomy has been described as a safe alternative to a thyroid lobectomy when involving an isolated cytologically indeterminate nodule in the isthmus (4-6). We present a case report describing our surgical approach to a solitary cytologically indeterminate thyroid nodule in the isthmus. We present the following article in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/aot-21-5).
Case presentation
A 48-year-old female was referred to surgery for an anterior cervical midline mass (Figure 1A,B). This caused compressive symptoms including dyspnoea when lying supine (Video 1). There was no history of neck radiation, or a family history of thyroid cancer. She noted a steady increase in the size of the nodule over the past year and had no previous neck masses in the past. Clinically she remained euthyroid with no excessive weight fluctuation or temperature intolerance. Her cervical neck examination revealed a midline swelling inferior to the thyroid cartilage and superior to the suprasternal notch which moved on deglutition and recorded on video. Cervical lymph nodes were clinically impalpable and she had no features of exophthalmos. Her heart rate was in sinus rhythm at 80 beats per minute.
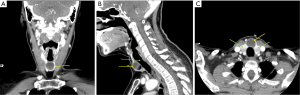
She was ascertained to be clinically and biochemically euthyroid. Imaging consisted of a thyroid ultrasound (US) and computerised tomography (CT) scan, both of which identified a cystic lesion isolated to the isthmus of the thyroid gland. The CT scan also excluded a thyroglossal cyst as the lesion moved on deglutition (Figure 2A,B,C). The lesion was a well-defined, hypoechoic cyst measuring 2.0 cm × 2.2 cm biaxially with no obvious cervical lymphadenopathy. The fine needle aspiration (FNA) cytology was non diagnostic due to insufficient follicular cells in the specimen.
Given the unique location of the nodule, as well as its increase in size, the concept of a thyroid isthmusectomy was discussed with the patient. She requested surgery for cosmetic reasons and found the nodule to be quite uncomfortable and unsightly. She was referred to a senior surgical colleague with extensive experience in thyroid surgery for a second opinion. The senior surgeon concurred with the surgical management of an isthmusectomy for the thyroid nodule. The patient consented to a thyroid isthmusectomy. She also understood that if her formal pathology report showed a thyroid malignancy, she would require a completion thyroidectomy with its attendant surgical risk and complications.
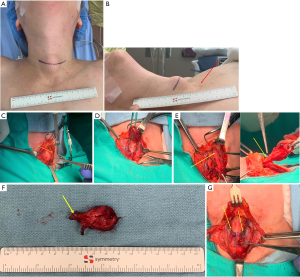
The surgical approach was similar to a routine thyroid lobectomy with a horizontal skin incision 2 cm superior to the suprasternal notch between the medial borders of bilateral sternocleidomastoid muscles (Figure 3A,B). The strap muscles were mobilised and the thyroid isthmus nodule visualized (Figure 3C). The nodule was excised off the trachea along with the pyramidal lobe and sent for pathology (Figure 3D,E,F). The lateral edges of the nodule were excised from the left and right thyroid lobes. The medial edges of both thyroid lobes were over-sewn with a 3-0 vicryl continuous suture to obtain adequate haemostasis (Figure 3G). The surgery was completed without incident. Pathology confirmed a benign nodule, and the patient’s post-operative recovery has been unremarkable. The patient expressed satisfaction with her surgical outcome and informed us that her respiratory symptoms have abated since the surgery. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Discussion
Thyroid nodules remain a common entity, with one study showing 67% of participants presenting with at least one incidental thyroid nodule on US imaging (7). The majority are benign but malignancy risk should still be ascertained. Radiological imaging is not the gold standard and pathological interpretation in the form of an US guided biopsy or thyroid lobectomy remains the standard bearer.
The precipitating factor when performing a thyroid lobectomy or isolated isthmusectomy for an isthmus nodule remains the malignant potential of the nodule. Studies have reported that the malignant nodules in the isthmus are more likely to invade adjacent tissues, such as the infrahyoid muscles and trachea (8). The pathophysiology of this invasion has not been clearly elucidated. If an isthmus nodule is malignant, appropriate surgical management would be a completion thyroidectomy. It is important to use clinical judgement to identify those at high risk for malignancy based on clinical findings, radiological imaging and a tissue biopsy.
Nodules isolated to the isthmus are quite rare, with an incidence of between 3% and 9% (9) compared to nodules in the right or left hemithyroid. Isolated thyroid isthmusectomy and thyroid lobectomy are safer options compared to a total thyroidectomy because the surgery is significantly less invasive and decreases the risks of trauma to the parathyroid glands as well as the recurrent and superior laryngeal nerves. Isthmusectomy has been shown to be effective in treating isolated isthmus nodules in the thyroid gland (10). The pyramidal lobe excision at the same time is significant as it reduces the difficulty of performing a completion thyroidectomy in the future if a diagnosis of thyroid malignancy is obtained.
The controversy arises in performing an isthmusectomy for a malignant nodule (6,11). The ability to obtain clear margins does not preclude a completion thyroidectomy. The decreased surgical risk has to be carefully weighed against the risk of a local recurrence when contemplating an isthmusectomy for a malignant nodule. Further evidence is required before altering the American Thyroid Association (ATA) guidelines.
In this case report, our patient had no risk factors for thyroid cancer. The pathology report described a benign appearing hyalinized thick-walled cyst, surrounded by normal thyroid parenchyma. Surgical excision was purely for her respiratory symptoms and cosmesis. The abatement of her symptoms justifies surgical management and obviates the need for a hemi thyroidectomy and its concomitant surgical risks.
Conclusions
There are currently no published guidelines outlining the surgical approach to an isolated nodule in the isthmus of the thyroid gland. A thyroid isthmusectomy is a considerably safer surgical option for patients presenting with a benign isthmus nodule.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/aot-21-5
Peer Review File: Available at http://dx.doi.org/10.21037/aot-21-5
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot-21-5). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Qin CD, Saha S, Meacham R, et al. Surgical risk after unilateral lobectomy versus total thyroidectomy: A review of 47,434 patients. Surgery Curr Res 2014;4:208.
- Zakaria HM, Al Awad NA, Al Kreedes AS, et al. Recurrent laryngeal nerve injury in thyroid surgery. Oman Med J 2011;26:34-8. [Crossref] [PubMed]
- Maser C, Donovan P, Udelsman R. Thyroid isthmusectomy: a rarely used but simple, safe, and efficacious operation. J Am Coll Surg 2007;204:512-4. [Crossref] [PubMed]
- Cannon CR. Isthmusectomy: The Un-thyroidectomy. Otolaryngol Head Neck Surg 2011;145:151-P151. [Crossref]
- Nixon IJ, Palmer FL, Whitcher MM, et al. Thyroid isthmusectomy for well-differentiated thyroid cancer. Ann Surg Oncol 2011;18:767-70. [Crossref] [PubMed]
- Ezzat S, Sarti DA, Cain DR, Braunstein GD. Thyroid incidentalomas. Prevalence by palpation and ultrasonography. Arch Intern Med 1994;154:1838-40. [Crossref] [PubMed]
- Hahn SY, Han BK, Ko EY, et al. Ultrasound findings of papillary thyroid carcinoma originating in the isthmus: comparison with lobe-originating papillary thyroid carcinoma. AJR Am J Roentgenol 2014;203:637-42. [Crossref] [PubMed]
- Pontieri G, Urselli F, Peschi L, et al. Is the Isthmus Location an Additional Risk Factor for Indeterminate Thyroid Nodules? Case Report and Review of the Literature. Front Endocrinol (Lausanne) 2018;9:750. [Crossref] [PubMed]
- Pérez-Ruiz L, Ros-López S, Gudelis M, et al. Isthmectomy: a conservative operation for solitary nodule of the thyroid isthmus. Acta Chir Belg 2008;108:699-701. [Crossref] [PubMed]
- Park H, Harries V, McGill MR, et al. Isthmusectomy in selected patients with well-differentiated thyroid carcinoma. Head Neck 2020;42:43-9. [Crossref] [PubMed]
Cite this article as: Pillay Y, Asefa R. Thyroid isthmusectomy for a benign nodule of the thyroid isthmus, a case report. Ann Thyroid 2021;6:4.



