Benign lateral aberrant thyroid—first case report in Hong Kong
Highlight box
Key findings
• Benign lateral aberrant thyroid does exist.
What is known and what is new?
• Diagnosis of a benign lateral aberrant thyroid, albeit rare, should be kept in mind when approaching and evaluating a neck mass.
What is the implication, and what should change now?
• USG + FNAC are recommended to be done for evaluation.
• Staged surgery is the preferred treatment option.
Introduction
Lateral aberrant thyroid is an archaic terminology that refers to thyroid tissue found in the lateral neck, which is anatomically separated from the orthotopic gland. It carries the connotation of malignancy since it was thought to be metastasis from thyroid carcinoma. This has been falsified by a few scattered published cases of benign lateral aberrant thyroid, including the following, the first reported case in Hong Kong. We present this case in accordance with the CARE reporting checklist (available at https://aot.amegroups.org/article/view/10.21037/aot-23-2/rc).
Case presentation
A 53-year-old gentleman with hypertension and obstructive sleep apnea complained of a painless progressively enlarging neck mass for months. Latest blood test showed a normal serum level of thyroid stimulating hormone at 0.96 µIU/mL.
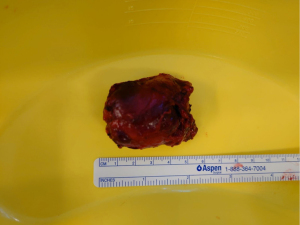
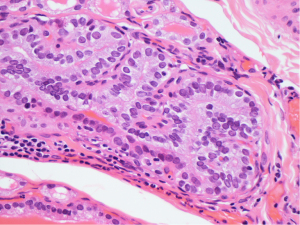
There was a 3 cm firm neck mass over the right level III region, otherwise, clinical examination of the head and neck region was unremarkable. Ultrasonography showed a hypoechoic mass with smooth border, deep to the sternocleidomastoid muscle. Fine needle aspiration cytology (FNAC) showed piece of thyroid tissue with colloid-containing thyroid follicles. These follicular cells are positive for thyroid transcription factor-1 (TTF-1) immunohistochemically (Figure 1).
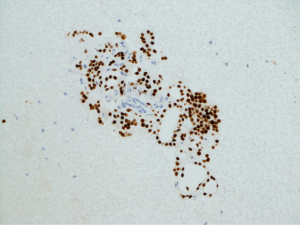
Computerised tomography (CT) scan of the neck depicted a well circumscribed neck mass with areas of hypodensity, which could be the result of necrosis or cystic change (Figures 2,3). There were several hypodense nodules, less than 1 cm in diameter over both lobes as shown by arrows. Orthotopic gland was otherwise normal in size.

In view of the progressively increasing neck mass, the patient was counselled for further imaging with positron emission tomography (PET)-CT in search of primary or definitive surgical treatment for pathological diagnosis. The patient opted for surgery. Meanwhile, further FNAC attempts were performed to the neck and to the ipsilateral thyroid respectively. The former one showed normal thyroid tissue whereas the latter was non-diagnostic.
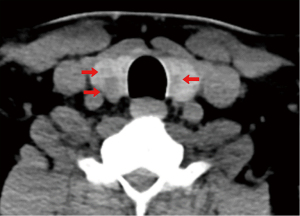
Right neck mass excision and right hemi-thyroidectomy was scheduled. Intraoperatively, the right neck mass (Figures 4,5) can be entirely separated from the thyroid gland. Frozen section of the neck mass came back with evidence of normal thyroid tissue and a benign lymph node. Additionally, there was a firm nodule over the right thyroid lobe.
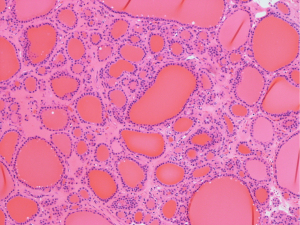
Normal thyroid tissue is demonstrated in the excised neck mass specimen (Figure 6). Pathology thus, confirmed the diagnosis of benign ectopic thyroid in the lateral neck region. There was an incidental T1b 10.1 mm papillary thyroid carcinoma with no lympho-vascular permeation or extra-thyroidal extension. Clear margin was obtained. Histologically, nuclear features of papillary thyroid carcinoma, with nuclear grooves and nuclear pseudo-inclusions are readily seen (Figure 7).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. In addition, the research has obtained approval from the cluster research ethics committee (REC Ref No. NTWC/REC/22084). Notice is also ready for review.
Discussion
Ectopic thyroid is a developmental abnormality, with a prevalence of 1 in 200,000 people. Most often, they are asymptomatic. Occasionally, patients may present with hypothyroidism and neck mass. Embryologically, thyroid gland is derived from a large median anlage and 2 lateral anlages. Lateral aberrant thyroid occurs when the lateral anlage fails to fuse with the median anlage at the 7th week of gestation. Lateral aberrant thyroid accounts for only 2% of all ectopic thyroid cases, yet they are generally perceived and treated as malignancy. There is one paper without cross referencing (Prado et al. 2012) (1), quoting a 12% rate of malignancy in lateral aberrant thyroid, which may underestimate the exact incidence because usually only rare benign cases are published.
A thorough review on the topics of benign lateral aberrant thyroid is summarised (Table 1). Different treatment plans were offered by respective authors, from medical treatment using levothyroxine supplementation to extensive total thyroidectomy with central and lateral neck dissection. Noteworthy is that a benign lateral aberrant thyroid in itself does not exclude presence of malignancy in the orthotopic thyroid gland. In fact, orthotopic thyroid gland is absent in 70% cases (5). As such, the role of preoperative ultrasound-guided (USG) would be of paramount importance, to search for primary malignancy, identify co-existing thyroid disorders, and to review the indication of thyroxine post-operatively.
Table 1
| References | Clinical exam | Management | Pathology of the thyroid (+/− LN) | Remarks | |
|---|---|---|---|---|---|
| Ectopic | Orthotopic | ||||
| Prado et al. 2012 (1) | 2 cm solid | Medical treatment with levothyroxine supplementation | N/A | N/A | Confirmed by 99mTc scintigraphy, followed up with FNAC |
| Otondi et al. 2020 (2) | 4.3 cm rubbery | Total thyroidectomy and neck mass excision | MNG | MNG | FS sent: benign thyroid tissue |
| Liu et al. 2022 (3) | 2 cm cystic | Total thyroidectomy, right lateral & central neck dissection | Benign (cysts) | MNG, 45 LNs −ve | FS of neck mass: no malignancy |
| Huang et al. 2021 (4) | N/A | Total thyroidectomy & bilateral central neck dissection | Benign | PTC, 3 LNs +ve | Bilateral PTC noted in USG and FNAC, postop RAI given |
LN, lymph node; N/A, not applicable; FNAC, fine needle aspiration cytology; MNG, multinodular goitre; FS, frozen section; PTC, papillary thyroid carcinoma; USG, ultrasound-guided; RAI, radioactive iodine therapy.
To avoid a diagnostic dilemma, a staged surgery would be favoured. Pathology can be reviewed following an en-bloc excision of the neck mass. If malignancy is confirmed, then a decision to proceed with an ipsilateral or total thyroidectomy with neck dissection can be discussed with patients. In addition to formulating diagnosis without repeated FNAC sessions as workup or during follow up, it also helps to avoid the operative risk of extensive surgical resection including neck dissection and in the same time, negate the need for lifelong thyroxine and/or calcium supplements.
Apart from the treatment of lateral aberrant thyroid, the proposed staged surgical approach can also be applied to management of thyroid ectopia in any part of the body, in gallbladder (6), anterior mediastinum (7), and even in the heart, in the right ventricle (8). Usually asymptomatic and noted as an incidental finding, thyroid ectopia may present as a growing lump with pressure symptoms. Imaging alone therefore has limited use. Regal et al. performed a midline partial sternotomy with en-bloc excision of a 5 cm mediastinal mass for diagnostic confirmation (7). On the other hand, Comajuan et al. also carried out an exploratory cardiac surgery with a tricuspid valve replacement after excision of an intracardiac mass (8). Histopathology eventually confirmed the diagnosis of ectopic thyroid tissue without evidence of malignancy in both cases. Subsequent workups in these cases included a targeted ultrasound of thyroid and thyroid function test, which was normal. Not surprisingly, the differential of thyroid ectopia was not included in both cases. Overall, thyroid ectopia indeed is a rare disease but should well be considered in the list of differential diagnosis. Preoperative ultrasound of the thyroid gland would facilitate the postoperative care of a patient when an ipsilateral or total thyroidectomy has to be discussed if malignancy is eventually confirmed. Overall, the proposed staged surgical approach could be applied in any cases of thyroid ectopia.
Conclusions
This case highlights the presence of a completely benign lateral aberrant thyroid. USG and FNAC are undeniably two important investigations that should be utilised preoperatively. A staged treatment approach is preferred to avoid potential surgical complications and the need for lifelong medication.
Acknowledgments
The histological and cytological slides were prepared by the Department of Clinical Pathology in Tuen Mun Hospital. Special thanks to Dr. Mak Siu Ming [MB, ChB, FHKCPath, FRCPA, FHKAM (Pathology), Department of Clinical Pathology, Tuen Mun Hospital, Hong Kong, China] for his efficiency and digital reproduction of the specimen slides.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aot.amegroups.org/article/view/10.21037/aot-23-2/rc
Peer Review File: Available at https://aot.amegroups.org/article/view/10.21037/aot-23-2/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.org/article/view/10.21037/aot-23-2/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal. In addition, the research has obtained approval from the cluster research ethics committee (REC Ref No. NTWC/REC/22084). Notice is also ready for review.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Prado H, Prado A, Castillo B. Lateral ectopic thyroid: a case diagnosed preoperatively. Ear Nose Throat J 2012;91:E14-8. [Crossref] [PubMed]
- Otondi CO, Cason FD, Kranc M, et al. Benign Ectopic Thyroid Tissue in the Neck: A Case Report of a Rare Finding. Cureus 2020;12:e7172. [Crossref] [PubMed]
- Liu GS, Berry GJ, Desai K, et al. Benign Ectopic Thyroid in the Lateral (Level II) Neck Compartment. Cureus 2022;14:e22140. [PubMed]
- Huang Q, Chen D, Ma Y. Bilateral papillary thyroid cancer with normal aberrant thyroid tissue. J Surg Case Rep 2021;2021:rjab578. [Crossref] [PubMed]
- Kumar Choudhury B, Kaimal Saikia U, Sarma D, et al. Dual ectopic thyroid with normally located thyroid: a case report. J Thyroid Res 2011;2011:159703. [Crossref] [PubMed]
- Kachare MB, Khandelwal A, Kulkarni SB, et al. Ectopic thyroid in duplicated gall bladder: a rare entity. Case report. Med Ultrason 2013;15:73-5. [Crossref] [PubMed]
- Regal M, Kamel MM, Alyami H, et al. Mediastinal ectopic thyroid mass with normal thyroid function and location: Case report. Int J Surg Case Rep 2018;52:5-7. [Crossref] [PubMed]
- Comajuan SM, Ayerbe JL, Ferrer BR, et al. An intracardiac ectopic thyroid mass. Eur J Echocardiogr 2009;10:704-6. [Crossref] [PubMed]
Cite this article as: Kwok JKS, Wong SCL, Yeung KW. Benign lateral aberrant thyroid—first case report in Hong Kong. Ann Thyroid 2023;8:10.