
Five-year review of incidental thyroid nodule management in the ENT outpatient department
Highlight box
Key findings
• Incidental thyroid nodules are heavily over investigated resulting in a substantial economic health care burden and undue patient anxiety.
What is known and what is new?
• There has been a recent increase in the observed incidence of small and micro thyroid cancers without a corresponding change in the thyroid cancer mortality rate demonstrating over-investigation.
• Our study shows poor compliance with British Thyroid Association guidelines in the management of these incidental thyroid nodules in our unit. We had 54 patients who had an incidental nodule demonstrated on computed tomography scan and after further ultrasound investigation with or without fine needle aspiration none demonstrated malignancy.
What is the implication, and what should change now?
• Stricter adherence with the guidelines will reduce over-investigation. Thorough radiology reports describing high risk features should be used alongside evaluation of clinical findings and risk factors to determine whether further investigation is required for incidental nodules.
Introduction
Incidental thyroid nodules are very commonly found with the increasing frequency of and advancements in medical imaging. Over-investigation results in a substantial economic health care burden and undue patient anxiety.
They can be detected in up to 20–67% of extrathyroidal ultrasound (US) examinations, for example, during US assessment of a neck for lymphadenopathy (1); in up to 25% of contrast enhanced computed tomography (CT) scan, such as during patient investigation for a lung malignancy; in up to 18% of magnetic resonance imaging (MRI) scans, including during MRI of cervical spine to assess degenerative or arthritic changes; and in 1–2.3% of positron emission tomography (PET) scans, for instance, during work up for an incurable non thyroid malignancy (1).
In some scenarios, reassurance with surveillance in primary care may suffice, but in others further evaluation based on clinical findings may be appropriate in the form of US investigation with or without fine needle aspiration (FNA). In other scenarios, for example, incidental nodules found on PET scan demonstrating widely disseminated non-thyroid cancers, any further evaluation may be inappropriate as it is unlikely to affect their quality of life or prognosis, even if a new thyroid cancer was detected.
The British Thyroid Association (BTA) guidelines states that incidental non-palpable nodules under 1 cm with no worrisome features (extra-capsular extension, tracheal invasion, associated lymphadenopathy) can be managed in primary care (2).
Our primary objective was to reduce over investigation of incidental thyroid nodules by the ENT Department in keeping with current BTA guidelines.
Our secondary objective was to assess the numbers of total thyroid cancers arising from incidental nodules. We present this article in accordance with the STROBE reporting checklist (available at https://aot.amegroups.com/article/view/10.21037/aot-23-17/rc).
Methods
Study design
We performed a retrospective analysis of all US thyroid examinations requested by the ENT outpatient department (OPD) over a 5-year period from 1st January 2014 to 31st December 2018. We examined the clinical information provided on every US thyroid request form the radiology department received in this timeframe. We confirmed that the nodules were incidental by analysing clinic letters and reviewing the initial imaging. We excluded any patients that were intentionally having an US for a symptomatic nodule, or having surveillance of a previously known nodule or goitre. We analysed clinic letters to assess if the nodule was reported as palpable. Radiological, cytological and histopathological data were analysed.
Setting
This study was performed in the Belfast Health and Social Care Trust. We only examined US thyroid requests from the ENT outpatient setting and excluded any requests from endocrine, general surgical or other medical departments.
Participants
We identified 614 individual patients having US thyroid of which 85 were for incidental thyroid nodules.
Outcome measures
For our primary objective we recorded size of the incidental nodule on the original imaging modality, the age of the patient and if adverse features were reported to see if the US scan was warranted or could have been avoided.
For our secondary outcomes we examined all cytological and histopathological specimens on electronic care records.
Ethical considerations
As the study was a clinical audit in order to produce information to inform delivery of a service or treatment already in use, the ethical approval was exempted and individual consent for this retrospective analysis was waived.
Results
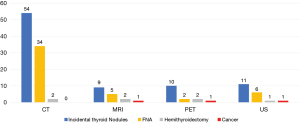
Overall, 85 out of 614 (14%) individual patients having US thyroid were for incidental nodules identified on imaging. Fifty-four incidental nodules were identified on CT, 9 on MRI, 10 on PET, 11 on US and 1 on chest X-ray.
In total, eight nodules were <1 cm without adverse features (six on CT, two on US) and had follow-up US requested. In all these eight cases there were no risk factors of thyroid cancer, and at all follow-up ENT clinics, the nodules were not palpable. These were therefore deemed as being over-investigated as per BTA guidelines (8/85=9.4%).
We found six nodules on CT, one on MRI and four nodules on US were between 1 and 1.49 cm. Twenty-six nodules on CT, three MRI, one PET and two US (32 nodules) were over 1.5 cm. In total, 34 nodule sizes were not specified in radiology report (although 74% >1.5 cm on follow-up US). We found six cases that required hemi-thyroidectomy. Of the 85 cases, 3 thyroid cancers were identified requiring completion thyroidectomy, all of which were over 1.5 cm (1 identified on MRI, 1 on PET, 1 on US) (Figure 1), and 4 follicular adenomas were identified on hemithyroidectomy (1 of which was between 1 and 1.5 cm and 3 >1.5 cm).
On the nodules identified on CT scan there was no specific comment on whether the nodule looked suspicious in 52/54 cases. It was reported as not suspicious in one case and reported suspicious in one case. On initial MRI no specific comment on whether the nodule looked suspicious was made in 8/9 cases and the nodule was reported as suspicious in 1/9 cases.
From our data 63.5% of incidental nodules identified were from CT scans. Interestingly, 0% of nodules on CT were cancerous. About 10% of our PET scan incidental nodules were cancerous.
Discussion
Incidental thyroid nodules are difficult to manage because despite having generally favourable mortality outcomes and indolent pathways, they are excessively reported on and investigated further to avoid the risk of missed cancer diagnosis.
Evidence suggests we are over investigating nodules as there has been a recent increase in the observed incidence of small and micro thyroid cancers without a corresponding change in the thyroid cancer mortality rate (3). Recent population-based studies estimate that the risk of malignancy in incidental thyroid nodules is 1.6% but studies in which incidental thyroid nodules undergo biopsy estimate that the risk at around 12%. There is often selection bias in these studies and the true rate is thought likely to be somewhere between these two rates (1). Our study found that 3.5% of the all the incidental thyroid nodules we investigated to be cancerous.
To best target over-investigated nodules, we assessed nodules that BTA guidelines suggest could be managed in primary care (2). These are the sub centimetre (cm) non palpable nodules with no worrisome features on CT. In our cohort we had at 8 (9.4%) patients that that met these criteria. According to BTA guidelines these could have been managed in primary care and not necessarily warranted further US investigation. This led to 13 US scans and 10 outpatient clinic appointments, and excess patient anxiety. We identified no cancers in incidental lesions under 1 cm so our data would suggest current BTA guidelines for management of incidental thyroid nodules to be safe. There were no hemithyroidectomy in these patients.
We may have, however, underreported the number of incidental nodules that we over-investigated, as further reading into the BTA guidelines states that “Incidentally detected nodules by CT should undergo clinical evaluation. In the majority of cases, no further assessment/investigation will be required. However, if there are suspicious findings on CT (extra-capsular extension, tracheal invasion, associated suspicious lymphadenopathy), or the patient belongs to a high-risk group or if there is significant clinical concern” (2). In the 54 cases we examined that were identified on CT scan, there were no reports suggesting extra-capsular extension, tracheal invasion or suspicious lymphadenopathy but one case reported suspicious calcification. We did, however, consider any nodule greater than 1cm to be of clinical concern, so we did not regard these as over-investigated for the purpose of this study.
American College of Radiology (ACR) guidelines suggests that for incidental nodules without any suspicious features identified on CT or MRI in the general population, if the patient is under 35 years old and the nodule is greater than 1 cm it requires further US evaluation, or if the patient is 35 years or older, then any nodule greater or equal to 1.5 cm requires further US evaluation (4). No further evaluation is required for nodules smaller than these sizes unless there are clinical risk factors for thyroid cancer. Extrapolating this guideline to our dataset, we had seven patients, all over 35 years old that had lesions between 1 and 1.5 cm, with no overt clinical risk factors for thyroid cancer and a non-palpable nodule that had further US investigation. This led to a total of 21 US slots and 22 outpatient clinic appointments that could be potentially avoided, and no cancers would have been missed. Also, one hemithyroidectomy would have been avoided out of seven total (14%) and no cancers would have been missed. A study comparing rates of malignancy from a three-tiered approach (age <35, aggressive imaging features, size >15 mm) against the common practice of investigating any nodule over 10 mm supports their guidelines. It concluded that a three-tiered approach almost halves the numbers of nodules requiring investigation (from 43% to 23%) while capturing the same proportion of thyroid malignancies and being no more likely to miss high-mortality malignancies. There was no difference in 10-year survival (3). We have compiled a table demonstrating the unnecessary investigations using ACR criteria compared to <1 cm incidental nodules in low-risk patients (Table 1).
Table 1
| Investigation | Using <1 cm non palpable incidental nodule in low-risk patient | Using ACR criteria* |
|---|---|---|
| Total number of patients over-investigated | 8 | 15 |
| Ultrasound scans | 13 | 21 |
| Outpatient clinic appointments | 10 | 22 |
| Fine needle aspirations | 5 | 9 |
| Hemithyroidectomies | 0 | 1 |
| Cancers identified | 0 | 0 |
*, ACR criteria states that in the absence of suspicious features on imaging, no US is required in low-risk patients if incidental nodule is <1 cm and the patient is <35 years old; or if the nodule is <1.5 cm and the patient is ≥35 years old. ACR, American College of Radiology; US, ultrasound.
Moving forward as a unit to further reduce over-investigation we should not consider a 1 cm size as a limit to request an US, but shall use it in co-ordination with clinical examination, assessment of risk factors and patients’ wishes to decide if further investigation is warranted for incidental nodules identified on CT or MRI. We must work alongside the radiology department to establish robust guidelines and a pathway for subsequent management to streamline and improve the service. We suggest a minimum dataset for reporting incidental nodules identified on CT and MRI scans, which should be included in all reports identifying incidental thyroid nodules: size of nodule, extra-capsular extension, tracheal invasion, calcification, associated lymphadenopathy. If there are no adverse features present and it is clinically non palpable then the radiologist could suggest no further intervention is required in the absence of risk factors (e.g., neck irradiation in childhood, endemic goitre, Hashimoto’s thyroiditis, family or personal history of thyroid adenoma, Cowden’s syndrome, familial adenomatous polyposis, familial thyroid cancer or obesity) (2). If there are clinically concerning features or risk factors the patient should be referred to ENT clinic for evaluation and discussion about whether further investigation is warranted.
In order to prevent the overtreatment of clinically insignificant micro-papillary carcinomas, if a nodule is <1 cm and has suspicious features that may warrant FNA based on certain US features (e.g., a solid hypoechoic nodule), we must make an informed decision based on whether there is any extrathyroidal extension or associated lymphadenopathy, or if the patient is high risk clinically before embarking upon FNA. Consultation with the multidisciplinary team should be sought (2).
In our study we had three cancerous nodules identified. One patient had an incidental U4 nodule identified on extrathyroidal US, one patient had a new goitre identified during MRI head and spine during work-up to exclude an inflammatory demyelination condition and one patient had a fluorodeoxyglucose (FDG) avid nodule on PET during assessment of myeloma. All three of these cases would have required investigation based on the BTA and ACR guidelines. We had four diagnostic hemithyroidectomies that did not show cancer. These cases be seen on Figure 1. Over our 5-year study the majority of our incidental nodules were identified on CT scan (63.5%) however 0% of these nodules were cancerous. Other studies suggest malignancy rates between of 0.5–9% on nodules identified CT scan (3).
With specific regards to incidental FDG avid nodules on PET scans the BTA guidelines state “Nodules detected by PET-CT with focal FDG activity should be investigated with US and fine needle aspiration cytology (FNAC), unless disseminated disease is identified and the prognosis from an alternative malignancy would preclude further investigation” (2). Other studies report there to be a risk of malignancy of less than 15%. An important concept in these patients is risk stratifying them based on their index malignancy, age and co-morbidities. If the patient is unlikely to survive 5 years based further investigation of the nodule may be inappropriate (5).
Pattison et al. found in their large retrospective study of 45,680 PET scans that they had 500 incidental thyroid nodules (1.1%) (6). They analysed 362 patients that met the inclusion criteria of having at least 12 months of clinical follow-up or confirmed death. They observed 180 deaths (50%) with a median survival of 20 months. The deaths were due to primary malignancy in 92.2% of cases or non-cancer-related death in 7.2% of cases. One patient died from an incidental medullary thyroid carcinoma (0.6%), but the authors were unsure if quicker intervention would have changed the outcome (6). Strong consideration should be taken for active surveillance in this cohort of patients given the guarded prognosis.
In our study, 10 patients had FDG avid nodules identified on PET scan, but none had disseminated disease or a significantly guarded prognosis on presentation to ENT, so we believe all warranted further investigation. Regardless of this 3/10 patients were deceased at 5 years. FNA was performed in 50% of the cases and two patients had hemithyroidectomy. There was one follicular adenoma and one follicular variant of papillary microcarcinoma. Overall, however, I think our department seemed very pragmatic and did not seem to inappropriately over investigate patients with significant life limiting disease.
Education of staff is a key component to reducing over-investigation of thyroid nodules. It will improve quality of radiology reports, which will promote less referrals from other departments and more appropriate investigation if it does arrive in the ENT Department. We have presented our data at local multi-departmental meetings to educate those requesting imaging when to investigate the incidental thyroid nodule.
There were a few limitations to our study. In the Belfast Trust, thyroid nodules can also be investigated by the Endocrine and General Surgical Department. We excluded their data as we wanted to audit our ENT outpatient service only. We therefore do not have a complete overview of all incidental thyroid nodules in the Trust. Also, our data only captures nodules that were investigated by US; it does not capture nodules that were not investigated after seen in the ENT outpatient clinic, or that were discharged after having US by another specialty/GP and not requiring referral to the ENT outpatient clinic.
Conclusions
Overall, we feel that it was a good study performed over a substantial time frame of 5 years, and our figures are in keeping with other studies. Following the BTA guidelines is an effective way of managing CT and MRI incidental thyroid nodules and stricter adherence to these guidelines will help streamline the ENT and radiology services. We believe this to applicable to all trusts in the National Health Service (NHS) that offer a thyroid service and that it if adopted will greatly reduce the economic health care burden and unnecessary anxiety caused by over investigation of incidental thyroid nodules.
Acknowledgments
Prize winning poster presentation at Irish Otolaryngology Head and Neck Society (IOC) 62nd Annual Conference October 2021.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aot.amegroups.com/article/view/10.21037/aot-23-17/rc
Data Sharing Statement: Available at https://aot.amegroups.com/article/view/10.21037/aot-23-17/dss
Peer Review File: Available at https://aot.amegroups.com/article/view/10.21037/aot-23-17/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.com/article/view/10.21037/aot-23-17/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. As the study was a clinical audit in order to produce information to inform delivery of a service or treatment already in use, the ethical approval was exempted and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fisher SB, Perrier ND. The incidental thyroid nodule. CA Cancer J Clin 2018;68:97-105. [Crossref] [PubMed]
- Perros P, Boelaert K, Colley S, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf) 2014;81:1-122. [Crossref] [PubMed]
- Nguyen XV, Choudhury KR, Eastwood JD, et al. Incidental thyroid nodules on CT: evaluation of 2 risk-categorization methods for work-up of nodules. AJNR Am J Neuroradiol 2013;34:1812-7. [Crossref] [PubMed]
- Hoang JK, Langer JE, Middleton WD, et al. Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee. J Am Coll Radiol 2015;12:143-50. [Crossref] [PubMed]
- Wadsley J, Balasubramanian SP, Madani G, et al. Consensus statement on the management of incidentally discovered FDG avid thyroid nodules in patients being investigated for other cancers. Clin Endocrinol (Oxf) 2023; Epub ahead of print. [Crossref] [PubMed]
- Pattison DA, Bozin M, Gorelik A, Hofman MS, Hicks RJ, Skandarajah A. 18F-FDG-Avid Thyroid Incidentalomas: The Importance of Contextual Interpretation. J Nucl Med 2018;59:749-55. [Crossref] [PubMed]
Cite this article as: McCrory D, Li C, Devlin B. Five-year review of incidental thyroid nodule management in the ENT outpatient department. Ann Thyroid 2023;8:12.


