
Obesity and thyroid cancer in Europe—is there a gender disparity developing?
Highlight box
Key findings
• The incidence of thyroid cancer in Europe is becoming marginally skewed towards the male population.
• The rise in obesity could be a contributing factor to the gender disparity seen in recent trends of thyroid cancer.
What is known and what is new?
• Obesity is a known source of morbidity and mortality worldwide contributing to significant burden rise globally, across various medical disciplines.
• Thyroid cancer is a cancer that is traditionally associated with the female population.
What is the implication, and what should change now?
• The implication is that more data and possible prospective cohorts should look further into obesity and thyroid cancer.
• Obesity and thyroid cancer awareness in men should be an important area to target for international associations.
Introduction
Background
The term “thyroid cancer” refers to a malignant tumor arising from thyroid tissue, either from follicular epithelial cells or the parafollicular C-cells of the thyroid. Research refers to a rapidly increasing incidence of thyroid cancer worldwide (1). The American Cancer Society (ACS) even states the rise in incidence is the highest compared to any other malignancy in the US. Currently, thyroid cancer ranks ninth in global incidence (2).
This could be attributed to variety of factors. Technological amelioration has surely played a role in earlier diagnosis, better prognostication, and perhaps better management. This includes advances in ultrasonography, cytology, interpretation and innovation (3). Nevertheless, many exogenous factors have been linked to contribute to the rise in incidence in the literature (4). These include iodine deficiency, radiation, diet, exposure to endocrine disrupting chemicals (EDCs), xenobiotics and environmental such as the correlation to highly volcanic areas.
Another notable common theme reported in similar observational surveys is a recent rise in thyroid cancer within the male population. Although thyroid cancer is traditionally and currently still more common in women, it tends to be more aggressive and morbid in men (5). Recent evidence, however, suggests that the rising incidence of thyroid cancer is affecting men at a much faster rate.
Two distinct cytopathological pathways are recognized, through well studied tumour progression models. There is a follicular lineage models, referred to as differentiated thyroid carcinomas (DTCs). This model revolves around a spectrum of differentiation, between a papillary histological subtype with distinct cytological identifying nuclear characteristics such as psammoma bodies, nuclear elongation and chromatin clearing, as well as margination and orphan-annie nuclei (6), as well as a follicular carcinoma variant that is perhaps less common and more aggressive. Both ends of the spectrum can furthermore progress into poorly differentiated histopathological subtypes, the worst prognostically referred to as anaplastic cell carcinoma. Medullary thyroid carcinoma follows a separate pathological lineage, that arises from the parafollicular C-cells of the thyroid (7).
With such an understanding of the pathophysiology of thyroid cancer, potential explanations to the rise in incidence, are being explored. Such studies utilize global collaboration studies to look at what the metrics of the rise, as well the temporal and geographic distribution of thyroid cancer incidence, mortality, and disability-adjusted life years. Unanimously and globally, these seem to follow an upstream trend, especially in areas of advancing sociodemographic index (SDI) and more western countries, possibly suggesting a correlation (8). While current such research already exists, this study aims to target a gap in the published literature, specifically tackling body mass index (BMI). Increasing evidence supports the role of estrogen pathways, diabetogenic carcino-antigens and insulin resistance in the development of thyroid cancer, amongst other risk factors (9). Utilizing the latest European data on the Global Burden of Disease (GBD 2019), this study interrogates BMI as a possible risk factor explaining the trend.
Studies focusing on BMI, question mostly its role behind the increase in incidence and exclude its effect on quality of life (10). This study focuses further on the morbidity attributed from obesity in thyroid cancer and looks at whether countries in Europe are being affected in an equal way, looking further into gender disparity within the data.
Objective
Primary aim
The primary aim of this study is to analyse European trends in change in thyroid cancer morbidity, specifically that attributed to high BMI. This study aims to statistically compare this between the male and female populations.
Secondary aims
The secondary aim of this study is to look at the extensive data from GBD 2019 in terms of European trends in thyroid cancer incidence, estimated rate of change and disability adjusted life years (DALYs), over both a geographical and temporal distribution within Western, Eastern and Central Europe, between 1990–2019.
Hypothesis
The hypothesis is that there was an increase in European thyroid cancer incidence as well as DALYs between 1990–2019, and that this has affected the male population more than the female population. The morbidity of thyroid cancer attributed to obesity in the male population is hypothesized to be higher than that in females. We present this article in accordance with the STROBE reporting checklist (available at https://aot.amegroups.com/article/view/10.21037/aot-24-24/rc).
Methods
Study design
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study does comply with the University of Edinburgh ethics standards. Due to the nature of the study, there was no requirement for specific individual review by the board, as no new personal data was used. Individual consent for this secondary analysis was waived.
This is a secondary cross sectional observational study, that investigates thyroid cancer data retrieved from GBD 2019. This is an extensive and comprehensive global observational epidemiological survey database, formulated by 8 global collaborators. It covers data relating to 369 diseases or injuries and 87 behavioral, environmental, and additional risk factor disease burdens for 204 countries and territories. It is based on multiple global data sources and employs a uniform and comparable methodology, considering age, year, sex, and other classifications. This database is the largest of its kind to date, and its data spans from 1990 to 2019 (11). Values of incidence, mortality, as well as DALYs attributed to thyroid cancer between the years from 1990 to 2019 were studied, for the countries and territories within Europe. This was done using the in-built Global Health Data query tool (GHDQT).
In GBD 2019, the definition of thyroid cancer corresponds to the International Classification of Diseases (ICD) codes: C73–C73.9, D09.3, D09.8, D34–D34.9, D44.0, Z85.850, 193–193.9, and 226–226.9. In total the study looks at 35 European countries, distributed geographically into Western, Central and Eastern Europe as defined by the pre-requisite database (12). SDI is a composite index of development status, strongly correlated with better health outcomes. Higher SDI countries tend to have higher rates of obesity. The methodology behind GBD 2019 have been previously published within the study itself (13,14).
Statistical analysis
Age-standardised incidence (ASI) was compared directly between Western, Eastern and Central Europe. This was separated and adjusted for sex and compared both collectively as well as subcategorized into individual country data. GBD 2019 data collected was data gathered between 1990 to 2019. To directly compare an estimate for the rate of change, the value peak percentages rate of change (PPRC) was calculated as below.
- Country with MAX ASI 2019 – Country with MAX ASI 1990
- Country with MAX ASI 1990
This was calculated for all the subgroups of data, i.e., for males and females separately attributed to either Western, Eastern and Central Europe.
Data on DALYs was further analysed more schematically using the statistical computing software R 4.3.3 (15). Individual trends of changes in DALY were first plotted similarly to those of ASI. Next the values for changes in DALY for thyroid cancer cases attributed to high BMI was extracted from the database individually and inputted onto a standard plot against time. This was done separately for men and women, as to assess for the rates of change by means of slope gradient calculation separately. All this data was standardized for age.
Individual trend line models were run in R 4.3.3 and compared to a best straight line that depicts a predictable trend line across the 30-year period. As the data published is observational in nature, a normality distribution analysis was underdone by means of a Shapiro-Wilk Normality test. Parametric tools of comparison are only appropriate if both datasets show normal distribution. Mean values from the data were compared statistically to a test equation adjusted to a normal distribution model as per Figure 1 above. Regarding the test, the null hypothesis is that there is no significant difference in mean DALY % between the two groups. The alternative hypothesis is a statistically significant difference in mean DALY % between the two groups.
The data was than analysed using a non-parametric Mann-Whitney U test to assess whether the variance between male and female mean trends of thyroid cancer DALYs attributed to BMI is statistically significant. A secondary non-parametric assessment was also undergone, using a Kruskal-Wallis test. This looked at statistical difference between the values for DALY attributes to BMI in Eastern, Central and Western Europe against each other.
Results
Summary of data
The study looks at data from the following 47 European countries: Albania, Andorra, Armenia, Austria, Azerbaijan, Belarus, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Georgia, Germany, Greece, Greenland, Hungary, Iceland, Ireland, Italy, Latvia, Lithuania, Luxembourg, Malta, Monaco, Montenegro, Netherlands, North Macedonia, Norway, Poland, Portugal, Republic of Moldova, Romania, Russian Federation, San Marino, Serbia, Slovakia, Slovenia, Spain, Sweden, Switzerland, Turkey, Ukraine. General summary exposure value (SEV) attribute from a high BMI was elevated in all the countries above when comparing data from 1990 to 2019, as per Figure 2.

General European epidemic trend of thyroid cancer
The overall ASI of thyroid cancer in Europe has increased from 3.07 per 100,000 people (2.95–3.17) in 1990, to an overall ASI of 3.84 per 100,000 people (3.48–4.26) in 2019, accounting for a rise of 25.08% when adjusted for both genders.
Stratified for gender, male ASI increased from 1.87 per 100,000 (1.62–1.96) to 2.67 per 100,000 (2.33–3.01) (+42.78%), while female ASI increased from 4.08 per 100,000 (3.93–4.25) to 4.92 per 10,000 (4.42–5.55) (+20.59%). The country with the highest ASI in 2019 was Iceland with an ASI of 8.48 per 10,000 (7.95–8.97) while the lowest recorded national ASI was that of Azerbaijan, 1.75 per 100,000 (1.37–2.23). The country with the highest ASI in 1990 was Iceland with a rate of 8.34 per 100,000 (7.44–9.39), and the lowest was that of Armenia, 0.79 per 100,000 (0.7–0.96). Figure 3 shows a detailed comparison between ASI rates of different countries. Figure 4 expresses the degree of variance as a colour-coded segment on the chart, for every country. Age standardized thyroid cancer in Europe has been generally rising throughout. As seen in Figure 5, ASI rates are still higher in the females than it is in males.



ASI trends for males
Within Eastern Europe, the peak incidence by country in males was Estonia for Eastern Europe in 1990, 1.35 per 100,000, while in 2019, it was Ukraine with 2.57 per 100,000. This represents an increase of +90.37%. The estimated peak percentage rate of change (PPRC) between the top incidence countries for Central Europe and Western Europe were +40.16% and +48.5% for males respectively (Czech Republic highest in 1990 with 2.45 per 100,000 and Montenegro highest in 2019, with 3.49) (Monaco highest both in 1990, with 6.34 per 100,000 and in 2019, with 9.42 per 100,000).
ASI trends for females
Female incidence of thyroid cancer follows a different trend. Eastern European estimated percentage rate of change (EPRC) was +36.79% for females (Lithuania in 1990 with 4.81 per 100,000 and Estonia in 2019 with 6.58 per 100,000). Central European EPRC for females was −18.56% (Czech Republic in 1990 with an ASI of 6.62 per 100,000, and Montenegro in 2019 with an ASI of 6.12). Western European EPRC for females was −35.01% (Iceland in 1990 with an ASI of 10.45 per 100,000 and Italy in 2019 with an ASI of 7.74 per 100,000). Figures 6-8 show the extrapolated data for individual countries.



Morbidity of thyroid cancer
Morbidity was evaluated by comparing trends of DALYs attributed to thyroid cancer, and how this adjusted to cases with high BMI. Concerning age standardized DALYs for females, a downward trend is seen in Western Europe. In the entire 30-year period, the average standardized value decreased from 18.59 DALYs per 100,000 to 11.49 DALYs per 100,000. This is congruent with values from Central Europe, that showed a drop from 23.77 DALYs per 100,000 to 13.89 DALYs per 100,000. Contrastingly, female DALY rates from Eastern Europe were shown to be rising, from 14.67 DALYs per 100,000 to 17.08 DALYs per 100,000.
Improvement rates in DALYs were less prominent in the male population. Western Europe reported an almost unchanged rate from 13.64 DALYs per 100,000 in 1990 to 11.88 DALYs per 100,000 in 2019. There was improvement in Central Europe, with rates dropping from 17.96 DALYs per 100,000 to 11.22 DALYs per 100,000. Eastern Europe showed a slight increase in DALY rates from 11.38 DALYs per 100,000 to 13.79 DALYs per 100,000. Figures 9,10 show this comparison graphically. DALY rates attributed to high BMI were plotted against time using R 4.3.3. All of these showed a positive upward trend, with the male trends being steeper than female trends throughout, as per Figure 11. This was also reflected as per P values in Table 1. It was tested for statistical significance as per the descriptives in Table 2.


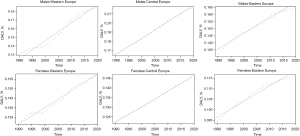
Table 1
| Category | P value |
|---|---|
| Central males | 0.002 |
| Central females | <0.001 |
| Eastern males | <0.001 |
| Eastern females | <0.001 |
| Western males | <0.001 |
| Western females | <0.001 |
DALY, disability adjusted life year; BMI, body mass index.
Table 2
| Gender | Region (Europe) | Mean DALY % | Overall mean DALY % |
|---|---|---|---|
| Male | Central | 0.19 | Males (C, E, W): 0.17 |
| Eastern | 0.16 | Females (C, E, W): 0.13 | |
| Western | 0.15 | ||
| Female | Central | 0.13 | Central (M, F): 0.16 |
| Eastern | 0.14 | Eastern (M, F): 0.15 | |
| Western | 0.11 | Western (M, F): 0.13 |
DALY, disability adjusted life year; C, Central; E, Eastern; W, Western; M, male; F, female.
Statistical analysis for normality, using Shapiro-Wilk Normality test, showed normality only in the Eastern male and female populations with P<0.01 and P=0.02 respectively, as per Table 3. This implies that direct comparison for statistical difference between male and female data cohorts had to be done by means of non-parametric data analyzes. Mann-Whitney U test performed showed low P values for Western, Central and Eastern Europe (P<0.001, P<0.001, P=0.04, respectively) (all region P<0.001). Kruskal-Wallis statistical analysis for assessment of statistical difference behind direct comparison of DALY rates attributed to BMI was also call statistically significant. These tests are depicted in Tables 4,5 respectively.
Table 3
| Category | P value |
|---|---|
| Males | 0.002 |
| Females | 0.002 |
| Central | <0.001 |
| Eastern | <0.001 |
| Western | <0.001 |
| Males Central | 0.13 |
| Males Eastern | 0.004 |
| Males Western | 0.09 |
| Females Central | 0.22 |
| Females Eastern | 0.02 |
| Females Western | 0.06 |
Table 4
| Mann-Whitney U test (males vs. females) | Test statistic value | P value |
|---|---|---|
| All regions | 769 | <0.001 |
| Central | 0 | <0.001 |
| Eastern | 309 | 0.04 |
| Western | 0 | <0.001 |
Table 5
| Kruskal-Wallis test (Central vs. Eastern vs. Western) | Test statistic value | P value |
|---|---|---|
| Both sexes | 28.33 | <0.001 |
| Males | 49.65 | <0.001 |
| Females | 67 | <0.001 |
Discussion
Age standardized incidence
The study shows an overall increase in European incidence of thyroid cancer. This is not evenly distributed geographically and between both genders. The country with the standout maxima ASI was always classically Iceland throughout the last 30 years. Most data attribute this explanation to the high volcanic activity environment. Interestingly nevertheless, Iceland was the country to show the steepest drop in standardized incidence over the past 10 years (16).
Eastern Europe showed the highest overall PPRC rates, both for males and for females. This reproduces a phenomenon evident in various other GBD 2019 as well as similar epidemiological studies on the topic. There seems to be correlation between national SDI and thyroid cancer incidence (17). This complies with the current take on modern pathophysiological hypotheses behind thyroid cancer, possibly explained by higher the rates of obesity, diabetes mellitus type 2, metabolic syndrome, and dyslipidemia.
In contrast to most other published observations, Central and Western European countries follow a different distribution. The increase in overall incidence was minimal in Central Europe and was even reversed in Western Europe. Notably, when the data are stratified between genders, an explanation is suggested for this trend. Thyroid cancer incidence seems to be decreasing for women but rising in men (18). EPRC values strongly re-enforce this idea. Western Europe shows a negative EPRC for females of −35.01%, compared to a positive +48.5% for males. Values are similar for Central Europe. In Eastern Europe, male and female ASI rates are also different, as suggested by EPRC values of +90.37% and +36.79% respectively.
Overall, this is congruent to the study hypothesis. Thyroid cancer is on the rise worldwide, with Europe being no exception. A malignancy historically affecting women more than men, is now affecting many more men, both in incidence and in quality of life. The second theme identified during this phase is the correlation with SDI. Countries in Central and Europe have always had a higher incidence of thyroid cancer than those in Eastern Europe, but this seems to be changing. With globalization, westernization, more processed diets and more food availability, thyroid cancer rates are also on the rise. The next phase of the study investigated these two themes further (19).
Morbidity and gender disparity
The overall morbidity and burden of obesity is universal in literature and effects every discipline of modern-day medicine (20-22). Data on morbidity were compared by measurement of DALYs. There is an overall downward trend in overall morbidity attributed to thyroid cancer over the last 30 years. This is likely multifactorial. There have been a lot of advances in thyroid surgery in general over the last 30 years, tackling earlier intervention, more detailed and safe surgical approaches with less post-operative complication rates. This likely plays a role the overall unsurprisingly decreasing morbidity of the diagnosis. This drop is also less evident in the standardized rates within Eastern Europe. Nevertheless, there is statistical evidence that this is affecting men worse than women as per the Mann-Whitney U test composed.
High BMI is a statistically significant risk factor for thyroid cancer within the extensive observational data cohort in GBD 2019. The results for DALY rates attributed to BMI plotted against time show that even though overall morbidity from thyroid cancer is on the decrease, the percentage of that morbidity attributed to obesity, is rising. This is notably skewed towards the male population with higher gradients in the slopes in all the three subcategories. Given that this is observational data, this statement needs to be investigated further. Possible suggestions for this would be prospective cohort studies comparing both focused groups, specifically comparing males with high BMI and control, hypothesizing to look at long term incidence of thyroid cancer. Thyroid cancer DALY rates attributed to BMI are shown to be consistently higher in men, and this is statistically significant both when comparing the male and female data against each other using the Mann-Whitney U test, as well as when comparing the three subcategories against each other, using Kruskal-Wallis (23).
Recent modern data are looking into explaining this phenomenon. The latest breakthrough has been by Zhang et al., in October 2023, where a systematic review identified eight distinct estrogen-related expressed genes (ERDEGs) that were directly associated statistically with thyroid tumor modulation, increase in immunological infiltration and poorer response to treatment (24). Tyrosine kinase inhibitors (TKIs), RET/PTC genes and BRAF mutations were all shown to be stimulated by estrogen as well, proposing an alternative pathway (25). There is an increasing focus within the world of public health onto adipose-endocrine associations and how obesity is leading to a hyperestrogenic state and multiple sequelae. Perhaps thyroid cancer could be another addition to this ever-growing list. Simultaneously, pharmaceutical advances regarding obesity management targets the study of glucagon like peptide 1-receptor agonists. These have been shown to increase the risk of thyroid cancer significantly (26,27).
Limitations
The study does not come without its limitations. The main limitation of the study is that the data itself is observational data. There is always risk of selection bias with no randomization, and no mention of standardized blinding. Secondly, the data is not stratified for subtypes of thyroid cancer. Thirdly, a potential confounding factor that the GBD 2019 database does not adjust for different ethnicity. A further suggestion is to compare the data across different grades of BMI and look at direct rates of morbidity rather than grouping them as DALYs. The study itself ranks as low to moderate risk of bias on the risk of bias in non- randomized tool for exposure (Robins-E) (28).
Conclusions
The European incidence of thyroid cancer has continued to increase over the past three decades. A gender discrepancy between the increase in rate of both incidence and morbidity of thyroid cancer does exist and is suggestive that males are being affected more. High BMI is an important attributable risk fact that deserves further awareness and greater attention, particularly in men and high SDI regions such as Western Europe.
The overall eneralizability of this study remains limited given the type of data, nevertheless this study could stem as a first oversight for further future research and further investigation. Furthermore, even though this study shows that men are being affected worse than women, when it comes to obesity associated thyroid cancer, further randomized control trials are required to obtain sufficient evidence to influence care.
Acknowledgments
The end project is a product of months of work, research, and learning. We would like to personally thank the University of Edinburgh for being given such an opportunity. First and foremost, this project would not be possible without the project supervisor. We would like to personally acknowledge and thank him for both helping through the ups and downs of this project, dedicating time for the project even after hours and during his personal free time. Secondly, we would also like to list our families who were a constant source of support throughout, both during the research project and throughout the entire Master’s project.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aot.amegroups.com/article/view/10.21037/aot-24-24/rc
Peer Review File: Available at https://aot.amegroups.com/article/view/10.21037/aot-24-24/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.com/article/view/10.21037/aot-24-24/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study does comply with the University of Edinburgh ethics standards. Due to the nature of the study, there was no requirement for specific individual review by the board as no new personal data was used. Individual consent for this secondary analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kitahara CM, Schneider AB. Epidemiology of Thyroid Cancer. Cancer Epidemiol Biomarkers Prev 2022;31:1284-97. [Crossref] [PubMed]
- Bao WQ, Zi H, Yuan QQ, et al. Global burden of thyroid cancer and its attributable risk factors in 204 countries and territories from 1990 to 2019. Thorac Cancer 2021;12:2494-503. [Crossref] [PubMed]
- Leenhardt L, Bernier MO, Boin-Pineau MH, et al. Advances in diagnostic practices affect thyroid cancer incidence in France. Eur J Endocrinol 2004;150:133-9. [Crossref] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. Erratum in: Lancet 2020;396:1562. [Crossref] [PubMed]
- Rahbari R, Zhang L, Kebebew E. Thyroid cancer gender disparity. Future Oncol 2010;6:1771-9. [Crossref] [PubMed]
- Al-Brahim N, Asa SL. Papillary thyroid carcinoma: an overview. Arch Pathol Lab Med 2006;130:1057-62. [Crossref] [PubMed]
- Shah JP. Thyroid carcinoma: epidemiology, histology, and diagnosis. Clin Adv Hematol Oncol 2015;13:3-6. [PubMed]
- Derwahl M, Nicula D. Estrogen and its role in thyroid cancer. Endocr Relat Cancer 2014;21:T273-83. [Crossref] [PubMed]
- Cho YA, Kim J. Thyroid cancer risk and smoking status: a meta-analysis. Cancer Causes Control 2014;25:1187-95. [Crossref] [PubMed]
- Zhao ZG, Guo XG, Ba CX, et al. Overweight, obesity and thyroid cancer risk: a meta-analysis of cohort studies. J Int Med Res 2012;40:2041-50. [Crossref] [PubMed]
- GBD Compare. (n.d.). Institute for Health Metrics and Evaluation. Retrieved May 1, 2024. Available online: https://vizhub.healthdata.org/gbd-compare
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. [Crossref] [PubMed]
- Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223-49. [Crossref] [PubMed]
- Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1160-203. [Crossref] [PubMed]
- Ripley BD. The R project in statistical computing. MSOR Connections 2001;1:23-5. [Crossref]
- Hrafnkelsson J, Tulinius H, Jonasson JG, et al. Papillary thyroid carcinoma in Iceland. A study of the occurrence in families and the coexistence of other primary tumours. Acta Oncol 1989;28:785-8. [Crossref] [PubMed]
- Maleki Z, Hassanzadeh J, Ghaem H. Correlation between socioeconomic indices and epidemiological indices of thyroid cancer from 1990 to 2019 year: a global ecologic study. BMC Cancer 2024;24:467. [Crossref] [PubMed]
- Leenhardt L, Grosclaude P, Chérié-Challine L, et al. Increased incidence of thyroid carcinoma in france: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid 2004;14:1056-60. [Crossref] [PubMed]
- Tang SD, Zi H, Tao H, et al. Secular trends of morbidity and mortality of thyroid cancer in five Asian countries from 1990 to 2019 and their predictions to 2035. Thorac Cancer 2023;14:3540-8. [Crossref] [PubMed]
- Gambardella C, Offi C, Romano RM, et al. Transcutaneous laryngeal ultrasonography: a reliable, non-invasive and inexpensive preoperative method in the evaluation of vocal cords motility-a prospective multicentric analysis on a large series and a literature review. Updates Surg 2020;72:885-92. [Crossref] [PubMed]
- Marotta V, Sciammarella C, Capasso M, et al. Germline Polymorphisms of the VEGF Pathway Predict Recurrence in Nonadvanced Differentiated Thyroid Cancer. J Clin Endocrinol Metab 2017;102:661-71. [PubMed]
- Pizza F, D'Antonio D, Lucido FS, et al. The Role of Ursodeoxycholic Acid (UDCA) in Cholelithiasis Management After One Anastomosis Gastric Bypass (OAGB) for Morbid Obesity: Results of a Monocentric Randomized Controlled Trial. Obes Surg 2020;30:4315-24. [Crossref] [PubMed]
- Yao CZ, Zhang M, Zeng YK, et al. Analysis and prediction of thyroid cancer morbidity and mortality trends in China. Zhonghua Liu Xing Bing Xue Za Zhi 2023;44:917-23. [PubMed]
- Zhang L, Zhou M, Gao X, et al. Estrogen-related genes for thyroid cancer prognosis, immune infiltration, staging, and drug sensitivity. BMC Cancer 2023;23:1048. [Crossref] [PubMed]
- Bailey WB, Cummings J. Statistics. Legare Street Press; 2023.
- Bezin J, Gouverneur A, Pénichon M, et al. GLP-1 Receptor Agonists and the Risk of Thyroid Cancer. Diabetes Care 2023;46:384-90. [Crossref] [PubMed]
- Silverii GA, Monami M, Gallo M, et al. Glucagon-like peptide-1 receptor agonists and risk of thyroid cancer: A systematic review and meta-analysis of randomized controlled trials. Diabetes Obes Metab 2024;26:891-900. [Crossref] [PubMed]
- Higgins JPT, Morgan RL, Rooney AA, et al. A tool to assess risk of bias in non-randomized follow-up studies of exposure effects (ROBINS-E). Environ Int 2024;186:108602. [Crossref] [PubMed]
Cite this article as: Borg L, Testa L, Camenzuli C. Obesity and thyroid cancer in Europe—is there a gender disparity developing? Ann Thyroid 2024;9:7.



