The intuitive da Vinci single port surgical system and feasibility of transoral thyroidectomy vestibular approach
Introduction
The transcervical approach is the gold standard technique for accessing the central neck in thyroid and parathyroid surgery; however, an anterior neck scar is inevitable (1). The presence of a central neck scar has been demonstrated to negatively impact patient quality of life (QOL) irrespective of scar severity (2-5).
Accordingly, remote-access approaches to the thyroid emerged to address the morbidity of the cervical incision. These approaches employ traditional endoscopic instruments as well as robotic surgical systems with documented efficacy and feasibility (6-9). Many of these approaches utilize dissection planes unfamiliar to traditional thyroid surgeons and are associated with increased costs, longer operative times, increased postoperative pain, technique-specific injuries, and a steep learning curve (10). Notably, these approaches are only able to displace the location of the cutaneous scar from the anterior neck to a less cosmetically conspicuous site. As a result, these techniques were slow to be adopted, especially in the West. In 2007, the New European Surgical Academy (NESA) proposed Transoral Thyroid Surgery as part of their natural orifice surgery project, which demonstrated that the central neck could be successfully accessed using a sublingual incision, sparking the development of novel thyroidectomy approaches (11-16). Subsequently, Wilhelm et al. performed a prospective proof-of-concept study on endoscopic minimally invasive thyroidectomy via the sublingual approach; this approach was ultimately abandoned due to associated serious complications such as severe tissue damage and increased conversion rate (17). In 2011, Richmon et al. described a tri-vestibular approach using a submental and subplatysmal approach (18,19). Later in 2015, Lee et al. published the first transoral robotic thyroidectomy series in four patients (20,21). Following this, Anuwong et al. published in 2016 the first case series of patients who underwent transoral endoscopic thyroidectomy vestibular approach (TOETVA) with excellent outcomes (22). The success of TOETVA has prompted many institutions around the world to adopt transoral vestibular approach (TOVA) using endoscopic or robotic surgical systems (8,23-31).
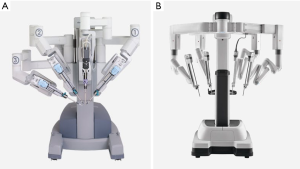
Robotic surgical systems offer theoretical advantages over endoscopic surgery, including 3D magnified visualization of the surgical field and increased dexterity with enhanced range of motion within the confined working space. In spite of this, endoscopic techniques have been more widely adapted than robotic surgical systems due to the high cost of operation, extensive learning curve, and technical limitations of robotic systems (32-34). For instance, a fourth accessory axillary incision is required when performing thyroidectomy with the da Vinci Si and Xi surgical systems (Intuitive, Inc., Sunnyvale, CA, USA) for counter-traction and drain insertion (35-37). Moreover, with the previous generation of the da Vinci robotic surgical system (Si and Xi), instrument movement is particularly unwieldly during dissection of the superior pole of the thyroid gland. As a result, an assistant familiar with the robotic system must be at the field to address arm collisions and camera positioning. In contrast, the new da Vinci single port (SP) robotic system has the capability of inserting 3 multi-jointed instruments in addition to a fully wristed 3DHD camera for high-definition visualization of the detailed anatomy of the surgical field through a 2.5 cm incision (Figure 1) (38). Therefore, the da Vinci SP system’s improved design may offer advantages in thyroid and parathyroid surgery. In this review article, we have provided a summary of existing literature on the SP system and its feasibility in the TOVA.
SP and transoral thyroid surgery vestibular approach in the literature
In 2018, the FDA approved the use of the da Vinci SP surgical system for SP urological procedures in adults. The following year, the FDA cleared the SP robot for radical tonsillectomy and tongue base resection. They stated, “The intuitive Surgical Endoscopic Instrument Control System (da Vinci SP Surgical System, Model SP1098) is intended to assist in the accurate control of Intuitive Surgical EndoWrist® SP Instruments during urologic surgical procedures that are appropriate for a SP approach and transoral otolaryngology surgical procedures in the oropharynx restricted to benign tumors and malignant tumors classified as T1 and T2…” (39). Because of limited FDA-approved indications for urological and oropharyngeal procedures, there is a paucity of original research on usage of the SP robot in endocrine procedures. Nonetheless, only three studies have explored the use of SP robot in performing the transoral thyroid surgery. Two studies were done on cadavers and the other is a 10-patient case-series. One of the studies done on cadavers is from our team and it demonstrates the preclinical feasibility study of SP surgical system in transoral thyroid surgery (40,41). The other preclinical study was conducted by Chan et al. and seeks to evaluate the next generation robotic system in transoral thyroidectomy (41). In addition, Park et al. published a case-series of 10 patients in South Korea who successfully underwent robotic transoral thyroid surgery using the da Vinci SP robotic surgical system (42).
Robotic surgical systems used in transoral thyroid surgery
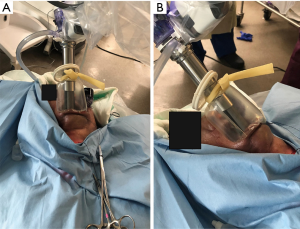
The da Vinci Si and Xi systems have previously been employed in the transoral thyroidectomy vestibular approach (Figure 2) (35). The da Vinci Xi was the latest generation utilized for transoral thyroid surgery, and consequently most reported cases employed the Xi system, which often requires an additional axillary incision. Unlike Si and Xi, The SP robotic system is a SP system containing a 25 mm cannula that allows for the passage of a full-wristed endoscopic 3DHD camera along with three multi-jointed EndoWrist® SP instruments, significantly increasing the viability of robotic surgery without the need for an axillary port. The EndoWrist® SP instruments have two additional degrees of freedom compared to previous generations, facilitating enhanced external and internal ranges of motion. This allows for more precise surgical control in narrow spaces. The location and axis of the camera in the SP system offers 360 degrees of rotation and can be adjusted through the surgeon console, obviating the necessity of a bedside assistant. Additionally, the endoscope of the SP is covered by an insulator, minimizing the risk of thermal damage to surrounding tissues.
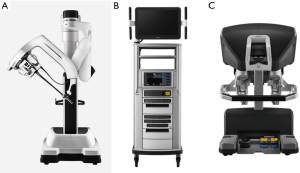
The da Vinci SP surgical system is made of three main components, similar to previous generations: the patient cart, the vision cart, and the surgeon console (Figure 3). Whereas the Xi system continues to utilize the 4-arm design, the SP is designed with only one arm with up to three flexible instruments that can emerge from this single arm (43).
Operative technique and the differences between SP and previous generations
In the preclinical study conducted by our group, we created the submental and subplatysmal space using laparoscopic instruments prior to docking the SP robot (patient cart), and CO2 gas insufflation was used to maintain the working space (33). In Chan et al., subplatysmal planes in the initial dissection were raised utilizing endoscopic guidance as in TOETVA. Then, a monopolar cautery and Kelly clamp forceps were employed to develop a plane over the periosteum of the mentum (41). Similar to Chen et al., the clinical study by Park et al. utilized monopolar cautery to create the working space with the midline incision measuring 25 mm prior to docking the robot (37).
In Park et al., following creation of the subplatysmal flap, a self-retaining retractor system was used instead of CO2 gas insufflation to maintain the working space. The patient cart containing the SP robot was docked perpendicular to the head of the surgical bed and the cannula was fixed 10 cm away from the midline incision. In both preclinical studies, CO2 gas insufflation was used to maintain the working space, similar to traditional TOVA. In our study, this was achieved by employing an Alexis (Applied Medical, Rancho Santa Margarita, CA, USA) wound retractor (XXS size) through the midline incision. The lower part of the Alexis was secured under the inferior edge of the mandible to prevent its slippage. Subsequently, we created a sealed tunnel between the working space and the SP cannula (located 6 cm from the inferior angle of the mandible) by tightly wrapping a Penrose drain around the upper end of the Alexis to prevent CO2 leakage and loss of the working space (Figure 4). A 30° endoscope was inserted through the upper slot while a ProGrasp Forceps, Maryland dissector and a monopolar curved scissors were inserted through the left, right and lower slots respectively in our study. On the other hand, in the study by Chan et al., two 5 mm cuts medial to the canines were made vertically to allow the placement of two trocars where a Maryland dissector and a hook cautery were used to create the working space deep to the platysma. The 5 mm port incisions were then closed to limit the gas leakage and an extra small wound protector (Applied Medical, Rancho Santa Margarita, CA, USA) was placed through the vestibular incision. In addition to the camera, three other instruments were used: the Maryland bipolar, fenestrated bipolar graspers, and monopolar scissors (41). Park et al. utilized only 2 incision ports (left side for Maryland forceps and the right for scissors) in addition to the camera. The transoral thyroidectomy is carried out in a similar fashion as endoscopic technique as described the literature as follows: (I) dissection of median raphe; (II) separation of strap muscles; (III) dividing the isthmus; (IV) upper pole dissection and ligation of the superior pedicle; (V) cephalocaudal dissection of the RLN; (VI) separation of the thyroid lobe off the trachea. Although the Harmonic (Harmonic Ace+, Ethicon Endo-Surgery, Cincinnati, OH, USA) is not currently included within EndoWrist SP instruments, our group successfully tried the endoscopic Harmonic HDI1000 through the lateral incision in addition to the three EndoWrist SP instruments to divide the median raphe, divide the isthmus and other steps where an energy device is typically used when performing TOETVA. Chan et al. described the use of a suction catheter through one of the ports if smoke occurs during the surgery. In addition to two EndoWrist instruments, Park YM et al. utilized a suction device and Maryland forceps inserted into the lateral incision through an endoscopic trocar that was controlled by the bedside assistant. Table 1 shows the differences between all three techniques.
Table 1
| Procedural steps | Preclinical study (1): Park et al. | Preclinical study (2): Chan et al. | Case-series: Park et al. |
|---|---|---|---|
| Creation of the working space | Laparoscopic as TOETVA | Endoscopic guidance as in TOETVA | Using monopolar cautery |
| Maintenance of the working space | CO2 gas insufflation secured by a tunnel made using Alexis wound retractor and Penrose drain | CO2 gas insufflation and maintained at a pressure of 6 mmHg | Self-retaining retractor instead of CO2 gas insufflation |
| Docking of the SP robot | 6 cm from the lower angle of mandible | 13 cm from the vestibular incision | 10 cm from the midline incision |
| Surgical technique | Harmonic ultrasonic shears were experimented via the lateral incisions to aid in dissection, cutting and sealing | A fenestrated bipolar was used to grasp the thyroid gland while Maryland bipolars and monopolar scissors were used to mobilize each hemi lobe of the thyroid | Only 2 robotic arms were utilized instead of 3, lateral vestibular incisions were utilized to insert suction device and Maryland forceps |
SP, single port; TOETVA, transoral endoscopic thyroidectomy vestibular approach.
Advantages and limitations of SP in transoral thyroid surgery
The advantages and limitations of SP robot in transoral thyroid surgery are summarized in Tables 2,3 respectively.
Table 2
| Easier docking |
| Suitable for narrow working spaces |
| Midline incision can take 3 instruments (6 mm each) in addition to the camera (8 mm) |
| Lateral incisions can be used for additional instruments controlled by the bedside assistant |
| Better ergonomics |
| Better visualization and full control of the camera from the surgeon’s console (except when cleaning is needed) |
| More flexible instruments (with 2 additional joints) |
SP, single port.
Table 3
| High cost of operation |
| Longer learning curve |
| Longer midline incision |
SP, single port.
Outcomes and perioperative complications
In the series by Park et al., all cases were completed successfully using the SP robot with a mean operative time of 177 min after SP robot docking, which required a mean of 47 minutes. No postoperative RLN injury or hypoparathyroidism were reported. Three out of ten patients complained of paresthesia along the cutaneous area supplied by the mental nerve, which resolved spontaneously within 1 month. All patients were extremely satisfied with the cosmetic outcome. Additionally, in both preclinical studies, thyroidectomy was completed successfully on human cadavers with preservation of parathyroid glands and recurrent laryngeal nerves.
Discussion
Over the last 3 decades proponents of minimally invasive surgery have touted the favorable surgical cosmesis in addition to potentially decreased postoperative pain, reduced length of hospital stay, and ultimately increased patient satisfaction with these procedures. While TOVA is not a minimally invasive surgery, some of the same benefits may apply (44). The introduction of the Davinci SP robot, with its advanced 3DHD camera and the versatile EndoWrist instruments, can potentially expand the selection criteria for transoral thyroid surgery to include patients with malignant nodules as well as those who might require concurrent central neck dissection. Thus, expanding these potential benefits to a greater patient population (45).
Robotic surgical systems, including the SP robot, however, have limitations that may continue to discourage widespread adoption. For instance, the cost of purchasing and maintenance is high compared to the cost of the traditional and laparoscopic techniques, limiting their availability to specialized institutions. Moreover, there is a steeper learning curve associated with robotic compared to endoscopic surgery (32,46). Furthermore, more studies are needed to evaluate mental nerve protection with use of the SP technique.
Although TOVA has proven to be safe and feasible, injury of the mental nerve is a technique-specific adverse event associated with TOVA. In TOETVA, a 15 mm midline incision is used compared to a 25 mm when using the SP robot. Further, as described in the study by Chan et al., at the end of the procedure the author noticed an increase of the vestibular incision to 35 mm. Despite this, there have been no reports of permanent mental nerve injury with the SP robot, although data is limited. In Park et al. however, only 2 instruments were used through the midline incision in addition to the camera, presumably to lower the risk of mental nerve injury. The author emphasized avoiding exceeding the premolar area when lifting the periosteal flap to stay away from the mental foremen and the main branch of the mental nerve. The mental foramen is positioned in line with longitudinal axis of the 2nd premolar tooth at the level of the vestibular fornix and about one finger breadth of the lower border of the mandible in 63% of individuals (47). Further studies are needed to evaluate the risk of mental nerve injury when performing transoral thyroid surgery and especially when making a larger incision then what is typically required with the solely endoscopic approach (48-50).
Conclusions
The SP robotic surgical system offers enhanced dexterity, while using a single central vestibular incision. Additionally, it allows for use a third robotic arm. These capabilities, when taken together, may increase the extent and complexity of thyroid surgery that may be performed via a vestibular approach. Limited evidence supports the widespread adoption of robots in thyroid surgery at this time.
Acknowledgments
Emerson Lee and Surya Khatri for technical editing.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jonathon Russell and Jeremy Richmon) for the series “The Management of Thyroid Tumors in 2021 and Beyond” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot-19-62). The series “The Management of Thyroid Tumors in 2021 and Beyond” was commissioned by the editorial office without any funding or sponsorship. JOR served as the unpaid Guest Editor of the series. RPT is a paid consultant for Medtronic and Hemostatix. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Latifi R, Rivera R, Gachabayov M, et al. Outcomes of 1,327 patients operated on through twelve multispecialty surgical volunteerism missions: A retrospective cohort study. Int J Surg 2018;60:15-21. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: A prospective cohort study. Int J Surg 2016;25:38-43. [Crossref] [PubMed]
- Best AR, Shipchandler TZ, Cordes SR. Midcervical scar satisfaction in thyroidectomy patients. Laryngoscope 2017;127:1247-52. [Crossref] [PubMed]
- Goldfarb M, Casillas J. Thyroid Cancer-Specific Quality of Life and Health-Related Quality of Life in Young Adult Thyroid Cancer Survivors. Thyroid 2016;26:923-32. [Crossref] [PubMed]
- Goswami S, Peipert BJ, Mongelli MN, et al. Clinical factors associated with worse quality-of-life scores in United States thyroid cancer survivors. Surgery 2019;166:69-74. [Crossref] [PubMed]
- Kandil EH, Noureldine SI, Yao L, et al. Robotic transaxillary thyroidectomy: an examination of the first one hundred cases. J Am Coll Surg 2012;214:558-64. [Crossref] [PubMed]
- Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000;10:1-4. [Crossref] [PubMed]
- Russell JO, Razavi CR, Al Khadem MG, et al. Anterior cervical incision-sparing thyroidectomy: Comparing retroauricular and transoral approaches. Laryngoscope Investig Otolaryngol 2018;3:409-14. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope 2011;121:1636-41. [Crossref] [PubMed]
- Berber E, Bernet V, Fahey TJ 3rd, et al. American Thyroid Association Statement on Remote-Access Thyroid Surgery. Thyroid 2016;26:331-7. [Crossref] [PubMed]
- Benhidjeb T, Burghardt J, Stark M. Novel technologies for natural orifice surgery: an overview. Minim Invasive Ther Allied Technol 2008;17:346-54. [Crossref] [PubMed]
- Benhidjeb T, Wilhelm T, Harlaar J, et al. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc 2009;23:1119-20. [Crossref] [PubMed]
- Benhidjeb T, Witzel K, Barlehner E, et al. The natural orifice surgery concept. Vision and rationale for a paradigm shift. Chirurg 2007;78:537-42. [Crossref] [PubMed]
- Stark M, Benhidjeb T. Natural Orifice Surgery: Transdouglas surgery--a new concept. JSLS 2008;12:295-8. [PubMed]
- Wilhelm T, Harlaar JJ, Kerver A, et al. Surgical anatomy of the floor of the oral cavity and the cervical spaces as a rationale for trans-oral, minimal-invasive endoscopic surgical procedures: results of anatomical studies. Eur Arch Otorhinolaryngol 2010;267:1285-90. [Crossref] [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Endoscopic minimally invasive thyroidectomy (eMIT): a prospective proof-of-concept study in humans. World J Surg 2011;35:543-51. [Crossref] [PubMed]
- Richmon JD, Holsinger FC, Kandil E, et al. Transoral robotic-assisted thyroidectomy with central neck dissection: preclinical cadaver feasibility study and proposed surgical technique. J Robot Surg 2011;5:279-82. [Crossref] [PubMed]
- Richmon JD, Pattani KM, Benhidjeb T, et al. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck 2011;33:330-3. [PubMed]
- Lee HY, Richmon JD, Walvekar RR, et al. Robotic transoral periosteal thyroidectomy (TOPOT): experience in two cadavers. J Laparoendosc Adv Surg Tech A 2015;25:139-42. [Crossref] [PubMed]
- Lee HY, You JY, Woo SU, et al. Transoral periosteal thyroidectomy: cadaver to human. Surg Endosc 2015;29:898-904. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Ahn JH, Yi JW. Transoral endoscopic thyroidectomy for thyroid carcinoma: outcomes and surgical completeness in 150 single-surgeon cases. Surg Endosc 2020;34:861-7. [PubMed]
- Anuwong A, Ketwong K, Jitpratoom P, et al. Safety and Outcomes of the Transoral Endoscopic Thyroidectomy Vestibular Approach. JAMA Surg 2018;153:21-7. [Crossref] [PubMed]
- Dionigi G, Lavazza M, Bacuzzi A, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA): From A to Z. Surg Technol Int 2017;30:103-12. [PubMed]
- Kadem SG, Habash SM, Jasim AH. Transoral Endoscopic Thyroidectomy via Vestibular Approach: A series of the first ten cases in Iraq. Sultan Qaboos Univ Med J 2019;19:e68-72. [Crossref] [PubMed]
- Park JO, Park YJ, Kim MR, et al. Gasless transoral endoscopic thyroidectomy vestibular approach (gasless TOETVA). Surg Endosc 2019;33:3034-9. [Crossref] [PubMed]
- Sivakumar T, Amizhthu RA. Transoral endoscopic total thyroidectomy vestibular approach: A case series and literature review. J Minim Access Surg 2018;14:118-23. [Crossref] [PubMed]
- Tesseroli MAS, Spagnol M, Sanabria A. Transoral endoscopic thyroidectomy by vestibular approach (TOETVA): initial experience in Brazil. Rev Col Bras Cir 2018;45:e1951. [Crossref] [PubMed]
- Yi JW, Yoon SG, Kim HS, et al. Transoral endoscopic surgery for papillary thyroid carcinoma: initial experiences of a single surgeon in South Korea. Ann Surg Treat Res 2018;95:73-9. [Crossref] [PubMed]
- Russell JO, Razavi CR, Shaear M, et al. Transoral Vestibular Thyroidectomy: Current State of Affairs and Considerations for the Future. J Clin Endocrinol Metab 2019;104:3779-84. [Crossref] [PubMed]
- Razavi CR, Khadem MGA, Fondong A, et al. Early outcomes in transoral vestibular thyroidectomy: Robotic versus endoscopic techniques. Head Neck 2018;40:2246-53. [Crossref] [PubMed]
- Russell JO, Clark J, Noureldine SI, et al. Transoral thyroidectomy and parathyroidectomy - A North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol 2017;71:75-80. [Crossref] [PubMed]
- Tae K, Lee DW, Song CM, et al. Early experience of transoral thyroidectomy: Comparison of robotic and endoscopic procedures. Head Neck 2019;41:730-8. [Crossref] [PubMed]
- Kim HK, Park D, Kim HY. Robotic transoral thyroidectomy: Total thyroidectomy and ipsilateral central neck dissection with da Vinci Xi Surgical System. Head Neck 2019;41:1536-40. [Crossref] [PubMed]
- Kim HK, Kim HY, Chai YJ, et al. Transoral Robotic Thyroidectomy: Comparison of Surgical Outcomes Between the da Vinci Xi and Si. Surg Laparosc Endosc Percutan Tech 2018;28:404-9. [Crossref] [PubMed]
- Kim HY, Chai YJ, Dionigi G, et al. Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surg Endosc 2018;32:688-94. [Crossref] [PubMed]
- Intutive da Vinci Surgical Systems. Da Vinci SP: For narrow access surgery. Available online: https://www.intuitive.com/en-us/products-and-services/da-vinci/systems
- FDA. The da Vinci SP surgical system; Indications for use. FDA. February 2019. Available online: https://www.accessdata.fda.gov/cdrh_docs/pdf18/K182371.pdf
- Park D, Shaear M, Chen YH, et al. Transoral robotic thyroidectomy on two human cadavers using the Intuitive da Vinci single port robotic surgical system and CO2 insufflation: Preclinical feasibility study. Head Neck 2019;41:4229-33. [Crossref] [PubMed]
- Chan JYK, Koh YW, Richmon J, et al. Transoral thyroidectomy with a next generation flexible robotic system: A feasibility study in a cadaveric model. Gland Surg 2019;8:644-7. [Crossref] [PubMed]
- Park YM, Kim DH, Moon YM, et al. Gasless transoral robotic thyroidectomy using the DaVinci SP system: Feasibility, safety, and operative technique. Oral Oncol 2019;95:136-42. [Crossref] [PubMed]
- Russell JO, Noureldine SI, Al Khadem MG, et al. Transoral robotic thyroidectomy: a preclinical feasibility study using the da Vinci Xi platform. J Robot Surg 2017;11:341-6. [Crossref] [PubMed]
- Zhang D, Caruso E, Sun H, et al. Classifying pain in transoral endoscopic thyroidectomy. J Endocrinol Invest 2019;42:1345-51. [Crossref] [PubMed]
- Zhang D, Park D, Sun H, et al. Indications, benefits and risks of transoral thyroidectomy. Best Pract Res Clin Endocrinol Metab 2019;33:101280. [Crossref] [PubMed]
- Razavi CR, Vasiliou E, Tufano RP, et al. Learning Curve for Transoral Endoscopic Thyroid Lobectomy. Otolaryngol Head Neck Surg 2018;159:625-9. [Crossref] [PubMed]
- Smajilagić A, Dilberovic F. Clinical and anatomy study of the human mental foramen. Bosn J Basic Med Sci 2004;4:15-23. [Crossref] [PubMed]
- Peng X, Li Z, Li H, et al. The clinical application of mental nerve dissection in transoral endoscopic thyroidectomy via an oral vestibular approach. Surg Endosc 2020;34:153-8. [Crossref] [PubMed]
- Zhang D, Fu Y, Dionigi G, et al. Human cadaveric model for studying the preservation of mental nerve during transoral endoscopic thyroidectomy. Surg Radiol Anat 2020;42:55-62. [Crossref] [PubMed]
- Yeh YT, Chen JY, Kuo PC, et al. Printing a Three-Dimensional Patient-Specific Safety Device for Reducing the Potential Risk of Mental Nerve Injury During Transoral Thyroidectomy. World J Surg 2020;44:371-7. [Crossref] [PubMed]
Cite this article as: Shaear M, Russell JO, Steck S, Liu RH, Chen LW, Razavi CR, Tufano RP. The intuitive da Vinci single port surgical system and feasibility of transoral thyroidectomy vestibular approach. Ann Thyroid 2020;5:20.